Introduction
Jaundice is the yellow colouring of skin and sclera caused by the accumulation of bilirubin in the skin and mucous membranes.
Neonatal jaundice occurs in 60% of term infants and 80% of preterm infants [1] and is caused by hyperbilirubinaemia that is unconjugated (divided into physiological or pathological) or conjugated (always pathological). High levels of unconjugated bilirubin have acute harmful effects as well as long term damage if left untreated, such as kernicterus.
10% of breast fed babies are jaundiced at 1 month.
Types of Jaundice
Physiological jaundice
Jaundice in a healthy baby, born at term, is normal and may result from:
- Increased red blood cell breakdown: in utero the fetus has a high concentration of Hb (to maximise oxygen exchange and delivery to the fetus) that breaks down releasing bilirubin as high Hb is no longer needed
- Immature liver not able to process high bilirubin concentrations
Starts at day 2-3, peaks day 5 and usually resolved by day 10. The baby remains well and does not require any intervention beyond routine neonatal care.
Physiological jaundice can progress to pathological jaundice if the baby is premature or there is increased red cell breakdown e.g. Extensive bruising or cephalohaematoma following instrumental delivery.
Pathological jaundice
Jaundice which requires treatment or further investigation.
- Haemolytic disease e.g. haemolytic disease of the newborn (rhesus), ABO incompatibility, G6PD deficiency, spherocytosis
- Onset less than 24 hours
- ?previous siblings treated for jaundice/family history/maternal rhesus status
- Maternal blood group (type O most likely to produce enough IgG antibodies to cause haemolysis)
- Requires investigation and treatment
- Bilirubin above phototherapy threshold
- Onset after 24 hours
- likely dehydrated ?breast fed baby establishing feeding
- increased haemolysis due to bruising/cephalohaematoma
- Unwell neonate: jaundice as a sign of congenital or post-natal infection
- Prolonged Jaundice: Jaundice for >14 days in term infants and 21 days in preterm, consider;
- Infection
- Metabolic: Hypothyroid/pituitarism, galactosaemia
- Breast milk jaundice: well baby, resolves between 1.5-4 months
- GI: biliary atresia, choledhocal cyst
Risk factors and history
Risk factors for pathological hyperbilirubinaemia: to be asked in history
- Prematurity, low birth weight, small for dates
- Previous sibling required phototherapy
- Exclusively breast fed
- Jaundice <24 hours
- Infant of diabetic mother
Clinical Presentation
- Colour: All babies should be checked for jaundice with the naked eye in bright, natural light (if possible). Examine the sclera, gums and blanche the skin. Do not rely on your visual inspection to estimate bilirubin levels, only to determine the presence or absence of jaundice.
- Drowsy: difficult to rouse, not waking for feeds, very short feeds
- Neurologically: altered muscle tone, seizures-needs immediate attention
- Other: signs of infection, poor urine output, abdominal mass/organomegaly, stool remains black/not changing colour
Investigations
Bilirubin
- Transcutaneous bilirubinometer (TCB) can be used in >35/40 gestation and >24 hours old for first measurement. TCB can be used for all subsequent measurements, providing the level remains <250 µmol/L and the child has not required treatment
- Serum bilirubin to be measured if <35/40 gestation, <24 hours old or TCB >250 µmol/L
- Infants that are not jaundice to the naked eye do not need routine bilirubin checking.
- Total and Conjugated Bilirubin is important if suspected; liver or biliary disorder, metabolic disorder, congenital infection or prolonged jaundice. Do not subtract conjugated from total to make management decisions for hyperbilirubinaemia.
Further investigations
- Serum bilirubin for all subsequent levels
- Blood group (Mother and Baby) and DCT
- FBC for haemoglobin and haematocrit
As needed
- U&Es if excessive weight loss/dehydrated
- Infection screen if unwell or <24 hours including Microbiological cultures if infection suspected: blood, urine, CSF. Consider TORCH screen.
- Glucose-6-phosphate dehydrogenase especially if Mediterranean or African origin
- LFTs if suspected hepatobiliary disorder
- TFTs
Management
Phototherapy
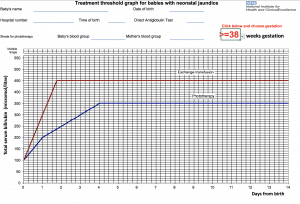
- Interpret bilirubin level using treatment threshold graphs that are gestation specific
- the more premature the infant the lower the level of bilirubin tolerated before neurological impairment
- Above: If level is on or above the phototherapy line for their gestation and age (in days) phototherapy should be initiated and bilirubin monitored
- Below: If level is below phototherapy line;
- >50µmol/L below, clinically well with no risk factors for neonatal jaundice do not routinely repeat level
- <50µmol/L below, clinically well repeat level within 18 hours (risk factors present) to 24 hours (no risk factors present)
- During:
- Repeat bilirubin 4-6 hours post initiation to ensure not still rising, 6-12 hourly once level is stable or reducing.
- NB. Maximum skin coverage, eye protection for babies, breaks for breastfeeding/nappy changes/cuddles to be coordinated to maximise phototherapy
- Stopping
- Stop phototherapy once level >50µmol/L below treatment line on the threshold graphs
- Check for rebound of hyperbilirubinaemia 12-18 hours after stopping phototherapy
Fluid intake
Do not give additional fluids with phototherapy unless indicated and if possible expressed maternal milk is preferred. If phototherapy intensified or feeding poorly consider NGT feeding or IV fluids.
Give consideration to underlying cause i.e. infection, biliary obstruction
Exchange Transfusion
This is the simultaneous exchange of the baby’s blood (hyperbilirubinaemic) with donated blood or plasma (normal levels of bilirubin) to prevent further bilirubin increase and decrease circulating levels of bilirubin.
Performed via umbilical artery or vein and is indicated when there are clinical features and signs of acute bilirubin encephalopathy or the level/rate of rise (>8.5µmol/L/hour) of bilirubin indicates necessity based on threshold graphs. This will require admission to an intensive care bed.
IV Immunglobulin
IVIG can be used as adjunct to intensified phototherapy in rhesus haemolytic disease or ABO haemolytic disease.
Complications
Kernicterus, billirubin-induced brain dysfunction, can result from neonatal jaundice. Bilirubin is neurotoxic and at high levels can accumulate in the CNS gray matter causing irreversible neurological damage. Depending on level of exposure, effects can range from clinically undetectable damage to severe brain damage.
Prognosis
Depends on underlying cause but if correctly and promptly treated prognosis is excellent.
Always refer to local trust guidelines.
References
| (1) | http://patient.info/doctor/neonatal-jaundice-pro |
| (2) | Jaundice in newborn babies under 28 days; NICE Clinical Guideline (May 2010) |
| (3) | Treatment threshold graphs https://www.nice.org.uk/guidance/cg98/evidence/treatment‐threshold‐graphs‐245372941 |
| (4) | Royal college of paediatric RCPCH guidelines for neonatal jaundice www.rcpch.ac.uk/…/Endorsed%20guidelines/Neonatal%20Jaundice/NICE%20Guideline |
Authors:
1st Author: Dr Phil Jordan
Senior Reviewer: Dr Umberto Piaggio