Introduction
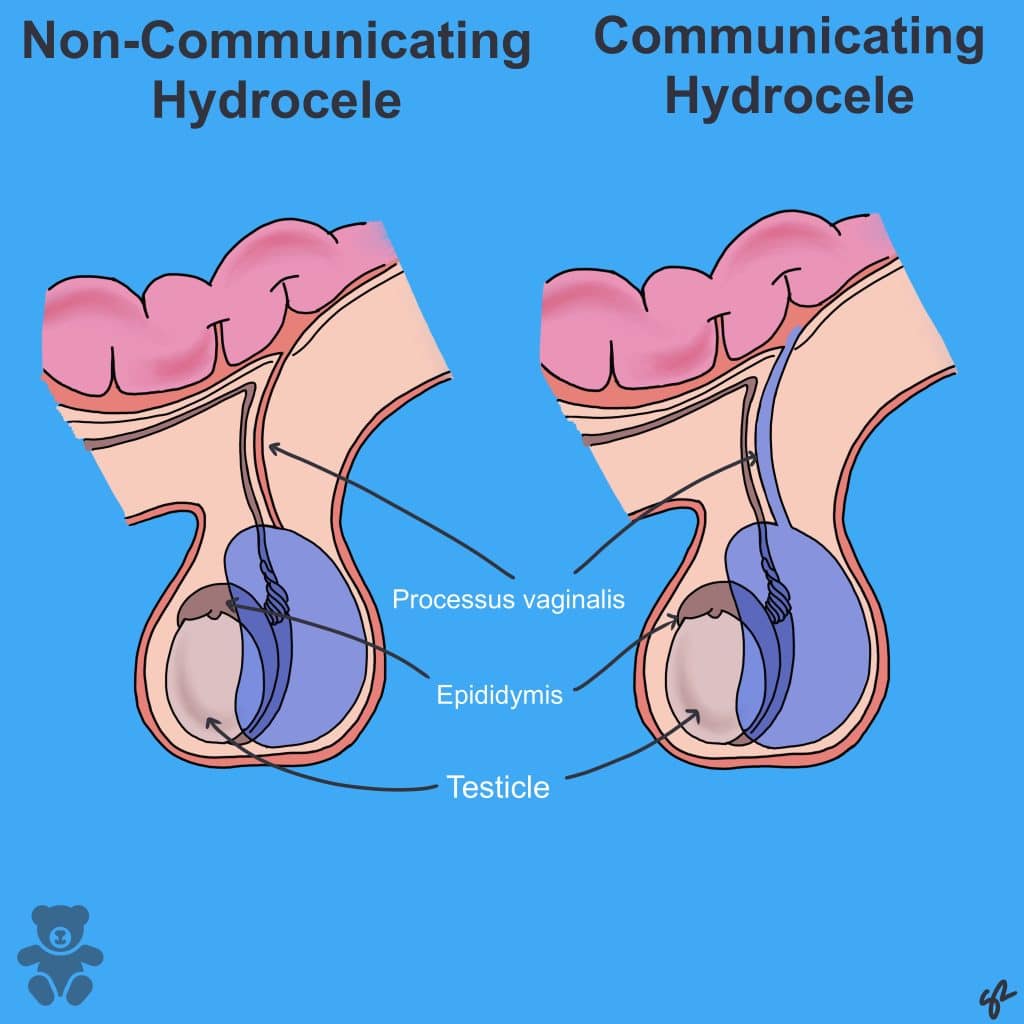
A hydrocele is a collection of fluid that builds up in the remnants of the processus vaginalis. It can either be communicating or non-communicating.
Pathophysiology
Communicating hydroceles occur due to the persistence of a patent processus vaginalis (PPV), allowing the free flow of peritoneal fluid from peritoneum to the tunica vaginalis (Fig 1). If the connection is large enough, an inguinal hernia may occur due to the protrusion of intra-abdominal contents.
Non-communicating hydroceles occur due to an imbalance between the production and absorption of serous fluid.
Aetiology
- Most paediatric hydroceles, seen in neonates and infants, are congenital.
- However, hydroceles presenting in older patients may be secondary to malignancy, testicular torsion, trauma or infection (e.g. epididymo-orchitis).
Clinical features
Patients present with a scrotal mass that is non-tender, smooth and transilluminates. There is notable scrotal enlargement following exertion.
Differential diagnosis
- Inguinal hernia: painless, inguinal/inguino-scrotal swelling, does not transilluminate, positive cough impulse, bowel sounds on auscultation
- Testicular cancer: often painless, occurs in older patients (20-40 years), solid/firm swelling that does not transilluminate
- Epididymitis: tender, often associated with erythema, pyrexia and urethral discharge
Investigations
Diagnosis is often clinical; however, an ultrasound scan can be used if there is uncertainty or to rule out any underlying pathology.
Management
- Reassurance: most hydroceles in neonates and infants resolve spontaneously and without complications by the first or second birthday.
- Surgery: open/laparoscopic PPV (patent processus vaginalis) ligation is offered electively to children in whom hydrocele persists beyond 2 years. Exploratory laparoscopy can be indicated if the hydrocele is large, infected, recurrent or to rule out secondary pathology.
References
| 1. | Newson L. Hydrocele. [Internet]. Patient.info. 2016 [cited 2 April 2021]. Available from: https://patient.info/doctor/hydrocele |
| 2. | Harding M. Lumps in the Groin and Scrotum. [Internet]. Patient.info. 2019 [cited 2 April 2021]. Available from: https://patient.info/doctor/lumps-in-the-groin-and-scrotum |
| 3. | Knott L. Epididymo-orchitis. [Internet]. Patient.info. 2016 [cited 2 April 2021]. Available from: https://patient.info/doctor/epididymo-orchitis-pro |
| 4. | Kogan B, Erdem E. Hydrocele – Symptoms, diagnosis and treatment [Internet]. BMJ Best Practice. 2021 [cited 2 April 2021]. Available from: https://bestpractice.bmj.com/topics/en-gb/1104 |