Introduction
Adrenal cortical insufficiency is a condition where there is insufficient secretion of cortisol from the adrenal gland. It can be either a primary problem i.e. within the adrenal cortex itself or a secondary problem, if there is insufficient ACTH secreted from the pituitary gland. It can also be due to prolonged ACTH suppression.
Physiology
Cortisol is regulated by the hypothalamic-pituitary-adrenal axis (HPA) as shown in figure [1]. Cortisol secretion is controlled via a negative feedback loop.
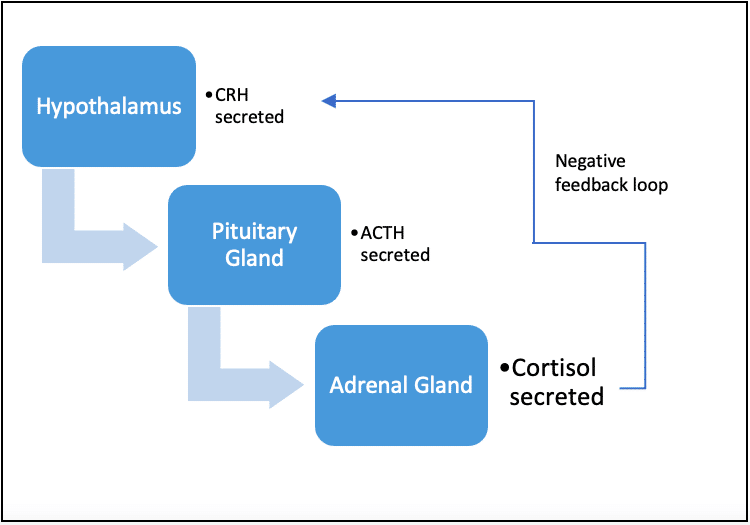
Figure [1] HPA axis demonstrating negative feedback action of cortisol on hypothalamus
Pathophysiology
Pituitary and adrenal problems can be:
- Genetic
- Traumatic
- Vascular
- Infective
- Tumour
- Autoimmune
- Iatrogenic
- Drugs
- Dexamethasone
- Surgery
Factors such as stress, illness can lead to increased cortisol secreted as part of the body’s fight or flight response.
Risk Factors
- High doses of steroids for prolonged periods, although can happen with more moderate doses
- Surgery to adrenal gland
- Radiation therapy
- Any pituitary insult
Clinical Features
History:
- Can be non-specific such as fatigue, vomiting, failure to thrive, weakness
- Specifically related to hypoglycaemia: pale, sweating, disorientated
- Specially related to hypotension: dizziness
- Specifically related to mineralocorticoid deficiency: collapse, weight loss, dizzy, craves salt
- Failure of genital development. Delayed puberty
Examination:
- Hyper-pigmented nails, mucus membranes, palmar creases
- Hypotension, tachycardia
Differential Diagnosis
Primary:
- Congenital Adrenal Hyperplasia: There is impaired cortisol synthesis due to enzyme deficiency mainly 21 hydroxylase but there are other rarer enzyme deficiencies in the steroidogenic pathway leading to hormone overproduction before this step. This generally leads to excessive virilization due to excess androgens and a salt wasting crisis. Babies can be born where gender is unclear or present at around 3-5 days of life in crisis with hyponatraemia, hyperkalaemia and hypotension. It can also present later in teenage years or early childhood with early puberty or evidence of androgen excess such as rapid growth, excess acne and early onset pubic hair.
- Congenital adrenal hypoplasia: either genetic such as DAX-1, SF-1 (other gene deficiency) or due to metabolic destruction such as Adrenoleucodystrophy or disorders of cholesterol synthesis such as Smith-Lemli-Optiz syndrome or StAR deficiency: occurs from birth with disorders of sexual development, collapse with hyponatraemia, hyperkalaemia and hypotension.
- Familial glucocorticoid deficiency: this is a selective failure to produce glucocorticoid only leading to hypoglycaemia, hypotension and electrolyte disturbance .
- Selective mineralocorticoid deficiency: this seen in some forms of CAH, but also aldosterone deficiency or inability to recognise aldosterone termed pseudohypoaldosteronism. This effects the salt pathway with hyponatraemia, hyperkalaemia and hypotension.
- Addison disease: there is destruction of the adrenal cortex which can be via infection, autoimmune. Typically presents insidiously with weakness, hyperpigmentation, fatigue, dizziness and salt craving.
- Autoimmune polyglandular syndromes 1,2,4: there are also features of other autoimmune conditions such as hypoparathyroidism, diabetes, vitiligo, coeliac disease.
Secondary
- Steroid withdrawal after prolonged use- this is most commonly seen in severe asthmatics on high doses of inhaled corticosteroids and sometimes oral steroids.
- Hypopituitarism
- Catastrophic infection or severe illness in PICU: leading to Waterhouse-Friderichsen syndrome and adrenal necrosis.
Investigations
- Synacthen test
- Cortisol/ACTH
- Insulin tolerance test
- Glucose
- U+Es
- Urine Steroid profile
- Aldosterone/ renin
Management
- Adequate fluid resuscitation if presenting in crisis with associated hypovolaemia and hypotension together with IM hydrocortisone
- Steroid replacement usually hydrocortisone. Fludrocortisone for any mineralocorticoid deficiency
- In the 1st year of life some babies require NaCl supplements.
- Sick day rules: increasing usual steroid dose to try and prevent addisonian crisis
- All patient need to carry emergency hydrocortisone as an intramuscular injection and display and medical alert bracelet to identify the condition in case of emergency.
Complications
- Addisonian crisis: a medical emergency which can develop in anyone who is dependent on steroids or unable to produce sufficient themselves. Can occur with intercurrent illness or stress as they are unable to increase the amount of steroid themselves in response. Presents with hypotension, collapse, confusion.
- Associated arrhythmias due to electrolyte disturbances, for example VF in very severe hyperkalemia
- In the neonatal period look out of disorders of sexual development.
- As a baby collapse and seizures, due to low glucose and hyponatraemia can be life threatening.
References
| No: | Reference: |
| 1 | Park J et al. Arch Dis in Childhood 2016;101:860-865. The diagnosis and treatment of adrenal insufficiency in childhood and adolescence. |
| 2 | Trapp CM et al. Congenital Adrenal Hyperplasia: an update in children. Curr Opin Endocrinol Diabetes Obes. 2011;18(3):166-170 |
| 3 | Strobel S et al. The Great Ormond Street Colour Handbook Paediatrics and Child Health. International Edition. Published by CRC Press 2007 |
