Introduction
Pierre Robin Sequence (PRS) is a rare syndrome within the paediatric population. It is the combination of a small lower jaw, cleft palate, and a tongue which is placed posteriorly within the mouth.
Epidemiology
PRS can occur either in isolation (20-40% of cases) or as part of a syndrome such as 22q11 deletion. Isolated PRS occurs in 1:5,000 births, whereas PRS as part of a syndrome can occur in 1:30,000 births. This is therefore much less common than the overall incidence of cleft lip or palate, which occurs in 1:700 births.
Pathophysiology
PRS is a sequence of events that occur in-utero, although the exact causes are not completely understood. Initially, the tongue is located between the two halves of the palate. At around 7-10 weeks of gestation, the lower jaw should undergo rapid growth, letting the tongue drop down and allowing the palate to fuse. If this does not occur, the tongue blocks this fusion and causes the palate to remain cleft. The tongue is also kept far back in the mouth, which leads to difficulties in breathing after birth.
Mutations near the SOX9 gene on chromosome 17 have been shown to be commonly associated with the development of PRS. The SOX9 protein is involved in tissue and organ development, in particular by regulating other genes that play a role in the development of the jaw and other parts of the skeleton.
Risk factors
- Genetic causes
- Oligohydramnios (reduced volume of amniotic fluid, limiting space for jaw growth)
- Connective tissue disease
- Myotonia (weakness) of the muscles in the face
Clinical features
Key features on examination
- Micrognathia: a disproportionately small lower jaw
- Cleft palate: a gap in the roof of the mouth
- Glossoptosis: a posteriorly placed tongue
- There may also be other signs which point towards an associated syndrome, (please see below).
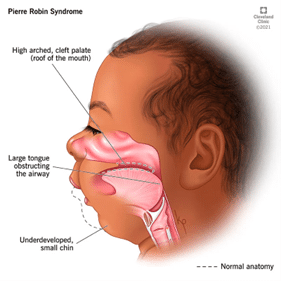
Figure 1: A diagram to show the physical clinical features of Pierre Robin Sequence (8).
Differential diagnosis
Associated syndromes and their common key features:
- Stickler syndrome: ‘distinctive facial features, eye abnormalities, hearing loss, and joint problems’ [4]
- CHARGE association: ‘Colobomas, Heart malformations, Atresia of the choanae, Retardation of growth and development (learning disability), Genital hypoplasia (in males), Ear abnormalities’ [7, p294]
- 2 deletion (DiGeorge syndrome): dysmorphism, velopharyngeal insufficiency and cleft palate, parathyroid hypoplasia, thymic hypoplasia, cardiac abnormalities, immunodeficiency
- Treacher Collins syndrome: maxillary hypoplasia, micrognathia, eye abnormalities, hearing loss

Figure 2: A man with Treacher Collins Syndrome. The characteristic maxillary hypoplasia and micrognathia can be seen (9).
Investigations
PRS can usually be detected on the 20 week anomaly ultrasound scan. If it is not picked up antenatally, the abnormal facial features should be seen on initial physical examination after birth. Investigations will then be needed to determine the extent of the abnormalities. These may include imaging, a bronchoscopy to look at the airway, and studies to assess the child’s sleeping and swallowing. If a syndromic cause is suspected, they should be referred to a geneticist for further investigation.
Management
Initial management
-
Breathing support
- Physical positioning should be tried initially. Babies with PRS should always sleep on their fronts, as this allows the tongue to fall forward, helping to unblock the airway.
- Nasopharyngeal airways can be used to maintain patency of the airway.
- In severe cases, intubation may be required. This may be a difficult airway situation and therefore full support should be gathered before attempting. These babies may require a tracheostomy.
-
Feeding support
- Babies with PRS usually need a special teet for bottle feeding, as their ability to suck and swallow is impaired.
- A feeding specialist should be involved to help guide the parents on how to optimize feeding.
Definitive and long-term management
- A child with PRS should be under a team that specialises in treating cleft palate or craniofacial disorders. One third of these children will undergo surgery before their first birthday.
- Surgical options that may be considered include:
- Glossopexy (tongue-lip adhesion) to open the airway
- Cleft palate repair
- Mandibular distraction to increase the size of the jaw
- Tracheostomy
- Feeding tube insertion
Complications
-
Airway complications
- Obstructive sleep apnoea
- Difficulties with intubation
- Aspiration
-
Feeding difficulties
- The cleft palate makes it impossible to separate the nose and mouth when drinking, so babies with PRS can’t breastfeed or use a normal baby bottle.
- A special bottle is needed, and they should be fed while either upright or lying on their side.
-
Malnutrition
- If the baby isn’t able to feed sufficiently using a special bottle, they may not be able to get all the nutrients they require.
- It may be necessary to insert a feeding tube, either via the nose or directly into the stomach.
-
Hearing difficulties
- A cleft palate can lead to middle ear effusions, causing hearing loss. If not treated, this can affect speech and language development.
- Grommets can be inserted into the eardrums during palate repair surgery, which will drain the effusions and treat the hearing loss until the function of the palate improves.
Prognosis
- The severity of PRS, and therefore the prognosis, varies greatly between children. The presence of an associated syndrome with PRS worsens prognosis, isolated PRS has a much better prognosis.
- Airway problems tend to gradually resolve over a few years as the mandible grows closer to its intended size. If this does not occur, mandibular distraction surgery may be necessary.
References
| 1 | Fox GF, Neonatology. In: Beattie M, Champion M (eds.), Essential Revision Notes in Paediatrics for the MRCPCH, 3rd edition, PasTest LTD, 2012, p295. |
| 2 | Genetic and Rare Diseases Information Centre. Pierre Robin sequence. Available from: https://rarediseases.info.nih.gov/diseases/4347/pierre-robin-sequence [Accessed 22nd November 2021]. |
| 3 | American Cleft Palate – Craniofacial Association. Pierre Robin Sequence. Factsheet available from: https://community.acpa-cpf.org/blogs/alexis-giannattasio/2019/01/03/acpa-publication-pierre-robin-sequence [Accessed 22nd November 2021]. |
| 4 | Genetic and Rare Diseases Information Center. Stickler syndrome. Available from: https://rarediseases.info.nih.gov/diseases/10782/stickler-syndrome [Accessed 22nd November 2021]. |
| 5 | Genetic and Rare Diseases Information Center. Treacher Collins syndrome. Available from: https://rarediseases.info.nih.gov/diseases/9124/treacher-collins-syndrome [Accessed 22nd November 2021]. |
| 6 | National Organization for Rare Disorders. Pierre Robin sequence. Available from: https://rarediseases.org/rare-diseases/pierre-robin-sequence/ [Accessed 22nd November 2021]. |
| 7 | Canham N, Genetics. In: Beattie M, Champion M (eds.), Essential Revision Notes in Paediatrics for the MRCPCH, 3rd edition, PasTest LTD, 2012, p294-295. |
| 8 | Cleveland Clinic. Pierre Robin Syndrome. Available from: https://my.clevelandclinic.org/health/diseases/21863-pierre-robin-syndrome [Accessed 30th December 2022]. |
| 9 | Children’s Craniofacial Association. Treacher Collins syndrome. Available from: https://ccakids.org/treacher-collins-syndrome.html [Accessed 30th December 2022]. |
| 10 | International 22q11.2 Foundation. Deletion vs. Duplication. Available from: https://22q.org/what-is-22q/deletion-vs-duplication/ [Accessed 30th December 2022]. |

