Introduction
Definitions1
Hyperthyroidism: excess production and secretion of thyroid hormones by the thyroid gland.
Thyrotoxicosis: the clinical manifestation of excess circulating thyroid hormones caused by hyperthyroidism or other causes (e.g. increased release of stored hormones from thyroiditis, increased ingestion of thyroid hormone medication)
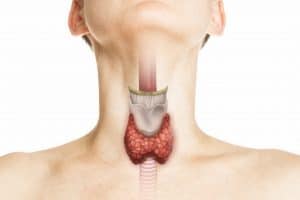
Figure 1: The thyroid gland is composed of two lobes that are connected by the central isthmus. It is positioned in the midline of the neck, anterior to the trachea and inferior to the thyroid cartilage.
Epidemiology
Hyperthyroidism is a condition affecting the thyroid gland and is relatively uncommon in childhood and adolescence. Its prevalence is higher in girls and also increases with age.2 0.94 per 100,000 under 15 year old have thyrotoxicosis, and for 84% of them it is due to Graves’ disease.3 Although hyperthyroidism is more common with increasing age, neonatal thyrotoxicosis affects 1-2% of infants born to mothers with a history of autoimmune hyperthyroidism.4
Pathophysiology5,6
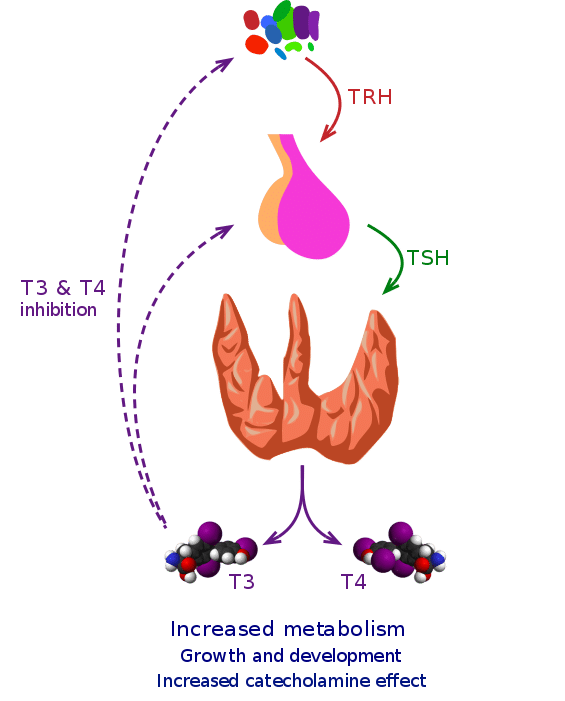
Hormonal axis
The hypothalamus-pituitary-thyroid (HPT) axis (Figure 2) is useful in understanding hyperthyroidism. The hypothalamus secretes Thyrotropin Releasing Hormone (TRH) which stimulates the anterior pituitary gland to release Thyroid Stimulating Hormone (TSH). TSH then binds to the TSH receptor (TSH-R) on the thyroid gland, stimulating the release of thyroid hormones T4 (thyroxine) and T3 (tri-iodothyronine) from the thyroid gland. To control the levels of circulating thyroid hormones, negative feedback is exerted by T4 and T3 onto the pituitary and hypothalamus, thus reducing the secretion of TRH and TSH.
Causes
Hyperthyroidism is usually due to problems with the thyroid gland (primary hyperthyroidism). It might rarely be due to increased levels of TSH (from abnormalities within the pituitary gland) which is known as secondary hyperthyroidism.7
The most common cause of hyperthyroidism is Graves’ disease. This is an autoimmune condition where antibodies (TSH receptor antibodies – TRAb) mimic TSH and activate the TSH-R on the thyroid gland, producing excessive thyroid hormone.
Other causes of hyperthyroidism include:
- Toxic multinodular goitre
- Toxic adenoma
- Thyroid carcinoma
- Neonatal hyperthyroidism – due to transplacental transfer of maternal TRAb to the foetus 8
- hCG-secreting tumours – hCG has a similar structure to TSH and so can mimic it 8
- Functioning pituitary adenoma leading to increased production of TSH
Risk factors7
- Family history of thyroid disease
- Personal or family history of autoimmune disease
- Increased iodine intake
- Smoking (especially for thyroid eye disease)
- Female
Clinical features
Thyroid hormone is essential for brain development, growth, and metabolism. Therefore, an imbalance of hormones can affect many systems in the body.
Symptoms: 2,4,5,8,9
- Weight loss / failure to thrive
- Increased appetite
- Rapid growth in height
- Sweating
- Heat intolerance
- Fatigue
- Anxiety, restlessness, irritability
- Diarrhoea
- Palpitations
- Warm, vasodilated peripheries
- Dyspnoea
- Insomnia
- Learning difficulties, behavioural problems, decreased concentration
- Deteriorating school performance
- Psychosis
- Delayed or accelerated puberty; oligo or amenorrhoea
Signs on examination5,8,9,10
- Goitre (bruit) that will move on swallowing but not on tongue protrusion (Figure 3)
- Fine tremor
- Hyperreflexia
- Moist, warm skin
- Tachycardia (rarely SVT), wide pulse pressure
- Proximal muscle wasting
- Hair loss
- Signs of thyroid eye disease – exophthalmos, ophthalmoplegia, lid retraction, lid lag (can cause dry eyes)
- Pretibial myxoedema – indicative of Graves’ disease
Differential diagnosis
- Non-hyperthyroid causes of thyrotoxicosis (e.g. transient thyroiditis) – check risk factors for thyroiditis (e.g. viral infection, drug induced), measure antibodies such as TRAbs and thyroid peroxidase antibodies (TPOAbs), consider radionuclide scanning or USS of the thyroid 1
- Hashimoto’s disease: causes hypothyroidism but initially it might cause a hyperthyroidism picture for a few weeks (hashitoxicosis) 8
- Eating disorder (e.g. anorexia): shares some similarities in presentation such as weight loss, fatigue, palpitations, hair loss, poor concentration etc. Bloods and thorough history needed 11
- Other causes of weight loss (e.g. diabetes mellitus, infection, anxiety) 12
- Phaeochromocytoma: increased adrenaline causes similar adrenergic symptoms but thyroid levels are normal 12
Investigations3
Laboratory tests
- Thyroid function tests (TFTs): T4 and/or T3 will be elevated, TSH will be suppressed (due to negative feedback)
- Antibodies: Thyroid peroxidase antibodies (TPOAb) and TSH receptor antibodies (TRAb).
- TPOAb may be present in both Graves’ and Hashimoto’s disease
- TRAb is indicative of Graves’ disease.
- Thyroglobulin antibodies (TgAb) are less commonly tested for, but can be raised in Hashimoto’s and sometimes also in Graves’.
Neonatal thyrotoxicosis: if the mother has Graves’ disease the baby will have TFTs done between day 5-14 to check their thyroid levels (timing may vary according to local practice) 13
Imaging or invasive tests
If hyperthyroidism is confirmed:
- USS of the thyroid: look for diffusely enlarged thyroid in Graves’ or focal enlargement in nodules
- Radionuclide thyroid scan: increased uptake in Graves’ disease, focal uptake in nodules, decreased uptake in thyroiditis (Figure 4)
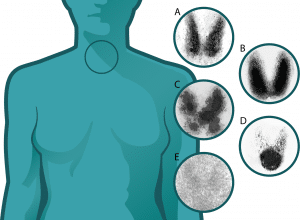
Figure 4: Radionuclide thyroid scan. A = normal thyroid B = Graves’ disease (diffuse increased uptake in both thyroid lobes) C = toxic multinodular goitre D = toxic adenoma E = thyroiditis (17)
Management
Initial management of Graves’ disease
1st line management is medical treatment with anti-thyroid drugs (ATDs). Carbimazole and propylthiouracil are the two options, but carbimazole is preferred due to the increased side effects of propylthiouracil in children. 10
There are also two methods to administer ATDs: 3
- Titration: dose of carbimazole is titrated to keep thyroid hormone levels within the normal range
- Block and replace: a higher dose of carbimazole is given to completely suppress the thyroid gland and then replacement levothyroxine is prescribed
NICE recommends titrating carbimazole for 2 years and then stopping the drug to see if they have gone into remission. Patients will also have lifelong monitoring. 1
Side effects of ATD: 3
- Minor: rashes, nausea, headaches
- Agranulocytosis
- Hepatitis
- Acute pancreatitis – discontinue permanently if this happens 1
Other considerations:
- For symptom relief, propranolol (beta-blocker) can also be given for the first few weeks until thyroid levels are controlled 3
- If thyroid eye disease is present, refer to ophthalmologist. The patient may need eye patches and artificial tears 4
Management of other causes: 1
- Neonatal hyperthyroidism: usually self-limiting within 1-3 months, might require treatment with propranolol or carbimazole 2
- Transient thyrotoxicosis without hyperthyroidism: only needs supportive management with beta-blockers
- Toxic nodules: treated the same as Graves’ disease
Definitive and long-term management
If medical treatment is ineffective or causing serious side effects, the patient has relapsed, or due to patient choice, they might be offered definitive treatment:
- Radioiodine therapy 3,6,10,14
- Given as a tablet or drink
- The iodine is taken up by the thyroid gland, and the radiation will destroy the thyroid cells
- Cure rates are 95% but sometimes requires a second dose
- Will need lifelong levothyroxine and monitoring due to subsequent hypothyroidism
- Not recommended for: <6 year olds, those with active thyroid eye disease, or those with severe uncontrolled hyperthyroidism (need to control medically first)
- Some restrictions for a few weeks after treatment (e.g. avoid contact with children due to radiation risk, so need to take time of school)
- Surgery 1,5,6,9,14
- Total thyroidectomy is the recommended surgical approach
- Subsequent hypothyroidism will need lifelong levothyroxine and monitoring
- Indications over radioiodine: very young children e.g. <6 years old, goitre, nodule, poorly controlled hyperthyroidism, suspicion of malignancy, want rapid cure
- Major complications occur in <2% of patients. Include: damage to parathyroid glands or recurrent laryngeal nerves causing hoarseness (rare with experienced thyroid surgeon)
Complications
- Thyroid storm (emergency) 3
- Presentation: fever, hyperthermia, tachycardia, hypertension leading to high output cardiac failure, GI dysfunction, CNS dysfunction and seizures
- Treatment: IV fluids, ATD (large doses of propylthiouracil +/- iodide), propranolol (minimise adrenergic effects), hydrocortisone (high risk of adrenal insufficiency), treat precipitating factor (e.g. infection)
- Side effect from treatment 3
- Agranulocytosis: report signs of infection (e.g. fever, sore throat). Check WBC and stop ATD
- Others: hepatitis, acute pancreatitis, hypothyroidism
- Thyroid eye disease: 1/3 children with thyrotoxicosis have significant eye disease which might not improve with treatment of the hyperthyroidism 3,9
- Complications of untreated hyperthyroidism 11
- Weight loss
- Hypercalcaemia 5
- Osteoporosis and fragility fractures
- Cardiovascular dysfunction, atrial fibrillation, embolic events
- Future pregnancies: antibodies that cause Graves’ disease can be passed onto the foetus even when treatment is no longer required, causing neonatal hyperthyroidism 14
Prognosis
After completion of ATD treatment, 40-75% relapse within 2 years. If this happens, patients can be treated with ATD again, or have radioiodine or surgery (lifelong thyroxine will be required after both procedures) 8
References
| No. | Reference |
| 1. | National Institute for Health and Care Excellence (NICE), Thyroid disease: assessment and management NICE Guideline [NG145]. [Internet]. 2019 [cited 8 April 2021]. Available from: https://www.nice.org.uk/guidance/ng145/chapter/recommendations#managing-thyrotoxicosis |
| 2. | Rodgers A, Salkind J. Endocrine system and growth. In: Xiu P, Datta S. (eds.) Crash Course Paediatrics. 5th ed. London: Elsevier; 2019. p.77-91 |
| 3. | Williamson S. Clinical Guideline: Medical management of children with thyrotoxicosis. [Internet]. 2014 [cited 8 April 2021]. Available from: https://www.speg.scot.nhs.uk/wp-content/uploads/2019/09/5.-SPEG-Childhood-Thyrotoxicosis-Guideline-v1.0.pdf |
| 4. | Thalange N, Beach R. Endocrinology and Metabolism. In: Kumar P, Clark M. (eds.) Essentials of Paediatrics. 2nd ed. London: Elsevier; 2012. p.144-145 |
| 5. | Qureshi Z, Tzaiferi V, Punniyakodi S, Emedo MJ, Bryant C. Endocrinology. In: Qureshi Z. (ed.) The Unofficial Guide to Paediatrics: Core Curriculum, OSCEs, clinical examinations, practical skills, 60+ clinical cases, 200+MCQs 1000+ high definition colour clinical photographs and illustrations. London: Qureshi Enterprises; 2017. p.205 |
| 6. | Butler G, Kirk J. Paediatric endocrinology and diabetes. Oxford University Press; 2020 Mar 10. |
| 7. | National Institute for Health and Care Excellence (NICE), Hyperthyroidism. [Internet]. 2021 [cited 8 April 2021]. Available from: https://cks.nice.org.uk/topics/hyperthyroidism/ |
| 8. | Albert D, Allen L, Alviani C, Bajaj Y, Choonara I, Coghill D, et al. Endocrinology. In: Tasker RC, Acerini CL, Holloway E, Shah A, Lillitos P. (eds.) Oxford Handbook of Paediatrics. 3rd ed. Oxford: Oxford University Press; 2021. p.405-465 |
| 9. | Dmitri P, Tinklin T. Diabetes and endocrinology. In: Lissauer T, Carroll W. (eds.). Illustrated textbook of paediatrics. 5th ed. London: Elsevier; 2018. p.453-471 |
| 10. | British thyroid foundation. Thyroid disorders a young person’s guide. [Internet]. 2019 [cited 8 April 2021]. Available from: https://www.btf-thyroid.org/Handlers/Download.ashx?IDMF=9c945c6f-ae9f-47f2-9c66-a62a95f1ab7d |
| 11. | Kahaly G, Bartalena L, Hegedüs L, Leenhardt L, Poppe K, Pearce S. 2018 European Thyroid Association Guideline for the Management of Graves’ Hyperthyroidism. Eur Thyroid J. 2018;7(4):167-186. Available from: https://doi.org/10.1159/000490384 |
| 12. | Newson L. Hyperthyroidism. [Internet]. 2020 [cited 8 April 2021]. Available from: https://patient.info/doctor/hyperthyroidism |
| 13. | Burren C. Guideline for the Management of Infant of Mother with Thyroid Disease. [Internet]. 2016 [cited 8 April 2021]. Available from: https://www.swneonatalnetwork.co.uk/media/89839/swnn-guideline-management-of-infant-of-mother-with-thyroid-disease-final-january-2016-version-03.pdf |
| 14. | American thyroid association. Hyperthyroidism in children and adolescents. [Internet]. 2018 [cited 8 April 2021]. Available from: https://www.thyroid.org/hyperthyroidism-children-adolescents/ |
| 15. | CFCF, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons [accessed 8 April 2021]. Available from: https://commons.wikimedia.org/wiki/File:Thyroid_vector.svg |
| 16. | CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons [accessed 8 April 2021]. Available from: https://commons.wikimedia.org/wiki/File:Struma_001.jpg |
| 17. | Maki G. Thyrotoxicosis and Pregnancy. PLoS Med. 2005;2(12):e370. Available from: https://doi.org/10.1371/journal.pmed.0020370.g002 |