Introduction
Psoriasis is a common, chronic, inflammatory condition affecting the skin. It can occur at any age, with about 1/3rd of cases developing before 20 years of age (1, 2).
Pathophysiology
The exact pathophysiology is unknown. It is thought to be multifactorial, with environmental, genetic, and immunological factors involved (3). There is T cell infiltration of the epidermis, secreting substances that activate the uncontrolled proliferation of keratinocytes. This means the skin cells proliferate around 10x faster than normal, which leads to characteristic thick and scaly plaque formation on the skin (2, 4).

Figure 1: Chronic plaque psoriasis on the extensor surface of the elbows.
Risk factors
Some risk factors for psoriasis flare include: (3)
- Infections (characteristically, streptococcal sore throat)
- Stress
- Mechanical injury (Koebner phenomenon*)
- Obesity
- Family history
- Drug induced
Psoriasis is NOT contagious (2)
*Koebner phenomenon is the appearance of new lesions on previously unaffected areas of skin, secondary to trauma (3)
Clinical features (2, 4, 5)
There are several different types of psoriasis that may be seen. These include:
- Chronic plaque psoriasis (the most common type overall)
- Guttate psoriasis
- Flexural psoriasis
- Scalp and facial psoriasis
- Pustular psoriasis
- Erythrodermic psoriasis
- Nail changes related to psoriasis e.g., ‘pitting’ appearance
Guttate, flexural and scalp/facial psoriasis are particularly common in children.
Clinical features from history
- Itchy
- Sore
- Burning
- There may be a family history present, history of an infection or of mechanical skin injury.
Clinical features from examination
Chronic plaque psoriasis:
- Raised inflamed patch of skin
- Thick silvery white scale
- Well defined lesion(s)
- Symmetrical distribution
- Auspitz sign*
*Auspitz sign is pin-point bleeding of the skin after a psoriatic scale is scratched/ lifted (6)
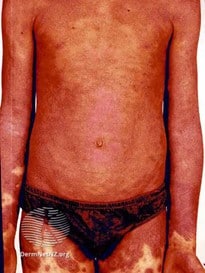
Guttate psoriasis:
- Small red plaques distributed across the torso
- Described as having a ‘raindrop’ appearance on the skin
- Often seen following infection

Figure 4: Guttate psoriasis on the trunk. The lesions resemble raindrops. (5)
Involvement can vary across different age groups:
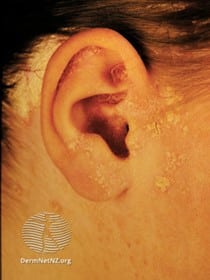
- In infants, involvement of the genital/nappy area is common.
- In young children, involvement of the scalp, face and flexural areas is common (e.g., arm and knee flexures).
- In older children, involvement of the face, ears and nails may be noted.
- In adolescents, elbows, knees, and scalp are typically involved.
Differential diagnosis
Juvenile psoriatic arthropathy (1)
- Inflammation and swelling of the joints. Skin and nail changes may be present.
Eczema (8)
- Eczema is typically seen in flexures, whereas typical psoriasis is seen on the extensors. This can be difficult to differentiate in flexural psoriasis.
- Itching is typically more intense with eczema than with psoriasis.
- Psoriasis is typically very well defined with a thick scale, whereas eczema is erythematous and may have excoriation marks, oozing blood or pus due to the intense itching.
- It is important to remember eczema and psoriasis can co-exist.
Lichen planus (9)
- Lichen planus typically presents with clusters of shiny, pink/purple papules. It may be itchy. There is also often oral involvement, affecting the inner cheeks and mouth.
Pityriasis rosea (10)
- Guttate psoriasis can mimic pityriasis rosea. This condition presents with small oval red patches mainly on the trunk, with an inner scale.
- A characteristic feature of pityriasis rosea is the presence of a ‘herald patch’ appearing 1-20 days before the generalized rash.
Investigations (2,5)
- Psoriasis is usually a clinical diagnosis.
- Sometimes, a skin biopsy may be needed to distinguish psoriasis from other similar conditions.
- A PASI (psoriasis area and severity index) score can be calculated to assess the severity and psychological impact of the condition, which helps guide management.
Management
There is no cure for psoriasis, however lots of treatment options are available.
Topical therapy: (6,11)
- Emollients
- Vitamin D analogues like calcipotriol
- Topical corticosteroids
- Dithranol
- Coal tar preparations e.g., shampoos (particularly useful for scalp psoriasis)
These would be first-line treatment options that may be offered by a GP. Further treatment options below would require referral to a specialist in dermatology or paediatrician.
Phototherapy (5)
- Ultraviolet light B (UVB) and PUVA (psoralen and ultraviolet light A) therapy to those >10 years of age for 6-12 weeks.
Methotrexate (5)
- Off label use, given once a week to those who have not responded to topical therapy and UV therapy. Regular blood tests are required.
Biologic therapy (5)
- Adalimumab and etanercept for those with severe, non-responsive psoriasis.
Complications
- Juvenile psoriatic arthritis
- Secondary skin infections
- Impact on quality of life including mental health problems (depression and anxiety)
Prognosis (5)
- Children with psoriasis may clear the condition completely, particularly if it was triggered by infection.
- Others may go on to have life-long chronic psoriasis.
- Psoriatic arthropathy is associated with worse prognosis.
References
| 1. | Pinson R, Sotoodian B, Loretta Fiorillo L. Psoriasis in children. Psoriasis: Targets and Therapy. 2016; 6:121-129. |
| 2. | British Association of Dermatologists. Psoriasis in children and young people. [Internet]. Bad.org.uk. 2020 [Accessed 6 March 2021]. |
| 3. | Kamiya K, Kishimoto M, Sugai J, Komine M, Ohtsuki M. Risk Factors for the Development of Psoriasis. International Journal of Molecular Sciences. 2019; 20(18):4347. |
| 4. | Rendon A, Schäkel K. Psoriasis Pathogenesis and Treatment. International Journal of Molecular Sciences. 2019; 20(6):1475. |
| 5. | Brown E. Paediatric psoriasis. DermNet NZ [Internet]. Dermnetnz.org. 2013 [Accessed 6 September 2021]. |
| 6. | Stanway A. Erythrodermic psoriasis. DermNet NZ [Internet]. Dermnetnz.org. 2004 [cited 6 March 2021]. Available from: https://dermnetnz.org/topics/erythrodermic-psoriasis/ |
| 7. | Hsu C. Global Dermatology. Psoriasis: Auspitz Sign [Internet]. Genevadermatology.ch. 2021 [Accessed 6 March 2021]. |
| 8. | Paller A. What’s the difference between eczema and psoriasis? [Internet]. Aad.org. 2021 [Accessed 21 October 2021] |
| 9. | British Association of Dermatologists. Lichen planus [Internet]. Bad.org.uk. 2021 [Accessed 6 March 2021]. |
| 10. | Oakley A. Pityriasis rosea. DermNet NZ [Internet]. Dermnetnz.org. 2014 [Accessed 6 March 2021]. |
| 11. | NICE. Psoriasis overview [Internet]. Pathways.nice.org.uk. 2021 [Accessed 6 September 2021]. |