Congenital heart defects (CHDs) are a group of structural abnormalities of the heart that are present at birth. They arise from disturbances in cardiac development during fetal life. Understanding the normal cardiac physiology is crucial to comprehending the pathophysiology of CHDs. This article provides an overview of cardiac physiology and explores its relation to different types of congenital heart defects.
Introduction
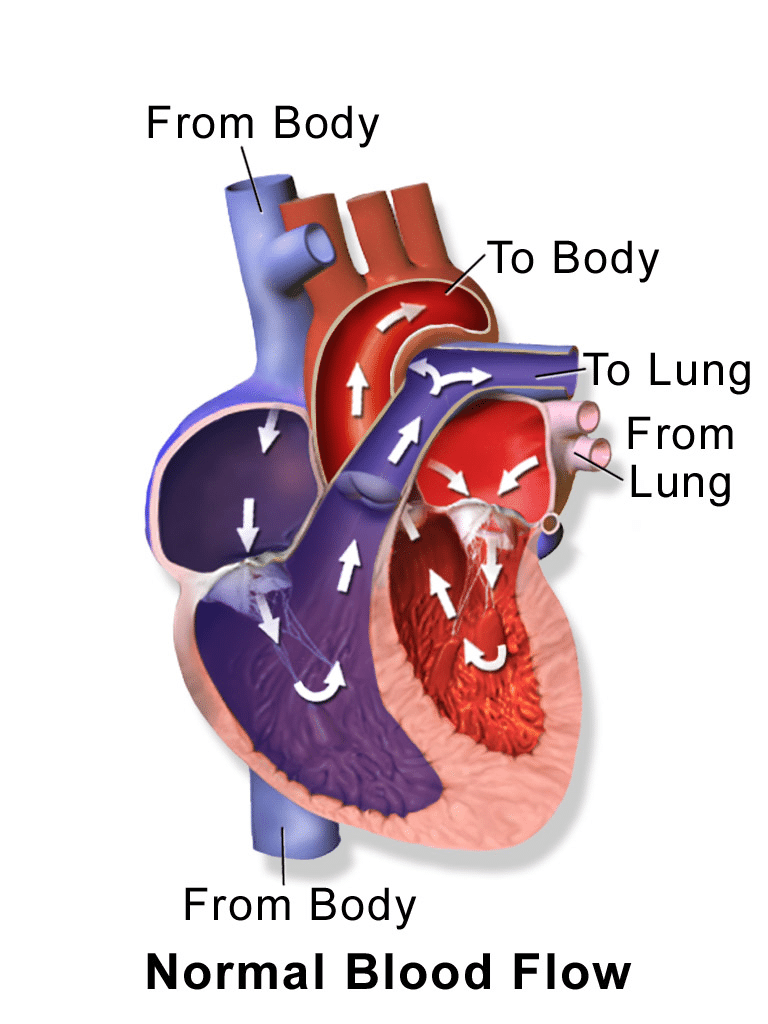
The heart is responsible for pumping blood throughout the body, providing oxygen and nutrients to the tissues. It consists of four chambers; A right and left atria, receiving blood returning from the body and lungs respectively, and a right and left ventricle pumping blood out to the pulmonary and systemic circulations respectively (Fig 1). Normal cardiac function relies on precise coordination between electrical, mechanical, and hemodynamic factors.
Cardiac cycle
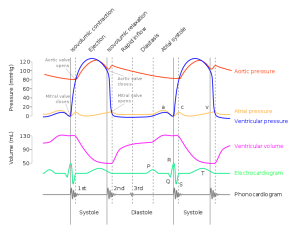
The cardiac cycle encompasses the events that occur from the initiation of one heartbeat to the beginning of the next. It is divided into two phases: diastole and systole. During diastole, the ventricles relax and passively fill with blood from the atria via the tricuspid (right) and mitral (left) valves. Towards the end of diastole, the atria contract (atrial systole) which completes the filling of the ventricles. During systole, ventricular contraction occurs, resulting in blood ejection into the pulmonary and systemic circulations via the pulmonary and aortic valves respectively. This cycle is regulated by electrical impulses generated by the sinoatrial (SA) node and propagated through the atria and ventricles via specialized conduction pathways (bundle of His). The electrical, mechanical, and pressure changes can be superimposed using the ‘Wiggers Diagram‘ (Fig 2). See our ‘ECG interpretation‘ article for more information on the electrical activity through the cardiac cycle.
Note:
Wave “a” = atrial contraction
Wave “c” = mitral valve bulging into the atrium after closure
Wave “v” = passive atrial filling.
Wave “P” = atrial depolarisation
Waves “QRS” = ventricular depolarisation
Wave “T” = ventricular repolarisation.
Types of Congenital Heart Defects
Congenital heart defects are classified into two main categories: cyanotic and acyanotic defects. Cyanotic defects cause a decrease in systemic oxygen saturation as the flow of blood tends to bypass the lungs, resulting in a bluish discoloration of the skin and mucous membranes (‘cyanosis’). Examples include tetralogy of Fallot, transposition of the great arteries, and tricuspid atresia. Conversely, acyanotic defects do not cause cyanosis and can be further categorized into shunt lesions and obstructive lesions.
Shunt lesions include ventricular septal defects, atrial septal defects, and patent ductus arteriosus. These result in abnormal blood flow between cardiac chambers, potentially causing volume overload to one or more chambers. This can cause pulmonary hypertension, congestive heart failure, and eventually, ‘right-to-left shunting‘, a reversal of the normal blood flow resulting in cyanosis.
Obstructive lesions create narrowing or blockages within the heart or great vessels, leading to increased pressure load on the affected chamber and subsequent hypertrophy. Over time, these conditions can result in compromised cardiac function and symptoms such as chest pain, fatigue, and shortness of breath. Obstructive lesions encompass coarctation of the aorta, pulmonary stenosis, and aortic stenosis.
Top Tip
Congenital Heart Defects can seem confusing at first. One method to help understand the anatomy and flow of blood is to visualise yourself as a red blood cell moving through the structures. Consider the defects and how they affect the pressure and flow of blood through the heart.
🩸
Impact on Cardiac Physiology
Cyanotic Congenital Heart Defects
As outlined above, cyanotic congenital heart defects are characterised by decreased systemic oxygen saturation, resulting in central and peripheral cyanosis. These defects significantly impact cardiac physiology and overall circulation.
In tetralogy of Fallot, there is a combination of four abnormalities: a ventricular septal defect, pulmonary stenosis, right ventricular hypertrophy, and an overriding aorta. The ventricular septal defect allows communication between the right and left ventricles. The degree of cyanosis (if any) is determined by the pressure difference between the left and right side. This is explored in more detail in our tetralogy of Fallot article.
Transposition of the great arteries involves a complete reversal of the connection of the aorta and pulmonary artery, leading to two separate parallel circulations. This defect requires mixing of oxygenated and deoxygenated blood at either the atria, ventricles, or through a patent ductus arteriosus prior to definitive management. This allows some oxygenated blood to reach the systemic circulation. However, the majority of blood returning to the right atrium bypasses the pulmonary circulation, leading to cyanosis.
Tricuspid atresia is characterised by the absence of the tricuspid valve, which separates the right atrium and right ventricle. There must be an inter-atrial connection to allow systemic venous return out of the heart via the left atrium and ventricle.
Acyanotic Shunt Lesions
As discussed previously, acyanotic shunt lesions include ventricular septal defects (VSDs), atrial septal defects (ASDs), and patent ductus arteriosus (PDA). Whilst these patients will often have normal systemic oxygen saturations, the haemodynamic effect over time of changes to the flow of blood through the heart can have significant consequences due to volume overload and chamber hypertrophy.
Ventricular septal defects involve an abnormal opening in the septum separating the two ventricles. This allows blood to flow from the left ventricle (higher pressure) to the right ventricle (lower pressure). As a result, there is increased blood flow to the pulmonary circulation, causing volume overload of the right ventricle. Over time, this can lead to right ventricular hypertrophy and pulmonary hypertension.
Atrial septal defects are characterized by an abnormal opening in the septum between the two atria. This allows blood to shunt from the left atrium (higher pressure) to the right atrium (lower pressure). The shunted blood then passes to the right ventricle and pulmonary circulation. Similar to VSDs, ASDs lead to increased blood flow to the lungs. Small ASDs may be asymptomatic and not lead to any further consequences, however large ASDs can cause volume overload of the right ventricle and potential right ventricular hypertrophy.
Patent ductus arteriosus is a condition where the fetal connection between the pulmonary artery and the aorta (ductus arteriosus) fails to close after birth. This results in a shunting of blood from the higher-pressure aorta to the lower-pressure pulmonary artery. The increased blood flow to the lungs leads to volume overload of the pulmonary circulation and can cause pulmonary hypertension.
Acyanotic Obstructive Lesions
Acyanotic obstructive lesions are characterised by narrowing or blockages within the heart or great vessels. These defects create pressure overload on the affected chamber and can significantly impact cardiac physiology and function. Examples of acyanotic obstructive lesions include coarctation of the aorta, pulmonary stenosis, and aortic stenosis.
Coarctation of the aorta is a narrowing of the aorta, usually near the insertion of the ductus arteriosus. This narrowing obstructs blood flow from the left ventricle to the systemic circulation, leading to increased pressure in the left ventricle and proximal aorta. The left ventricle becomes hypertrophied which compensates for a while, however this will lead to heart failure if left untreated.
Pulmonary stenosis refers to the narrowing of the pulmonary valve or the pulmonary artery, obstructing the blood flow from the right ventricle to the pulmonary circulation. This obstruction causes increased pressure load on the right ventricle, leading to right ventricular hypertrophy.
Aortic stenosis involves the narrowing of the aortic valve, which obstructs blood flow from the left ventricle into the systemic circulation. This obstruction leads to increased pressure in the left ventricle. Over time, the left ventricle will become hypertrophied but this will eventually weaken the muscle and lead to heart failure.
Summary
Congenital heart defects are a diverse group of structural abnormalities that affect the normal cardiac physiology. Understanding the intricate interplay between cardiac function and different types of defects is crucial for accurate diagnosis, appropriate management, and long-term care of individuals with CHDs. Ongoing research and advancements in medical technology continue to improve outcomes and offer hope to patients and their families.