Introduction
Children with Down Syndrome are a diverse population and there is a spectrum of features and associated disability. Named after Langden Down, who first identified the phenotype.1 It affects 1:1000 live births in the UK. The underlying cause is aneuploidy ‘Trisomy 21’ and it is this addition of genetic information (including the critical region 21q22.3) which disrupts expected development, producing the dysmorphic features and mild to severe cognitive impairment. It is the most common chromosomal abnormality in the UK; the prevalence however remains static since 1989 due to selective terminations of approximately 90% of antenatal diagnoses.2
Genetics
Ninety-five percent of Down Syndrome is a result of trisomy 21, where there are extra copies of chromosome 21 in each cell. Instead of having the normal 46 chromosomes, there are 47, as demonstrated in Figure 1. This abnormality occurs sporadically during the cell cycle. In a small amount of cases (3.5%) additional chromosomal material is inherited from one of the parents, who carries a “balanced translocation” including chromosome 21. Even more infrequently it may be secondary to mosaicism, where there is a mixture of some cells containing 3 forms of chromosome 21, while others are typical with 46 in total. Occasionally in these individuals, a milder phenotype is expressed, however this is variable.3
Risk Factors
There is evidence that sporadic mutations are associated with maternal maturity, for example at 35 years the risk is 1:270, jumping to 1:50 at >45 years.4
Antenatal Screening
The majority of Down Syndrome diagnoses will be identified on antenatal screening. A combination test, including biochemical markers in maternal blood (10-14+1 wks) and nuchal translucency on ultrasound scan (11+2-14+1 wks), provides a pre-test probability. A quadruple test is offered to women presenting from the second trimester onwards. If there is a risk of >1:150 invasive diagnostic tests are offered in the form on chorionic villi sampling (<13 wks) or amniocentesis (>15 wks). These carry a 1% risk of miscarriage.5
The UK Government has recently approved a new antenatal diagnostic test with a specificity and sensitivity superior to the current mode of testing, at near 100%.6 This measures cell-free foetal DNA (cffDNA) present in maternal blood. This can be done earlier and with the hope of preventing the need for invasive and risky diagnostic testing later in pregnancy.
Clinical Features
Down syndrome diagnoses are also identified postnatally either due to declined/missed antenatal screening or false negatives (2%). These babies may be identified by dysmorphic features- see Figure 2.

Fig 2. The typical dysmorphic features seen in a patient with Down Syndrome.
Down syndrome is associated with the following conditions, and it is their increased incidence which dictates initial management and subsequent health surveillance. These are detailed according to system:
●Visual problems – congenital cataract, infantile glaucoma, strabismus and nystagmus.
●Hearing difficulties – predominantly conductive hearing loss.
●Ear, Nose and Throat – small upper airway spaces cause increased risk of infections, particularly glue ear. Preponderance to obstructive sleep apnoea (OSA), with the subsequent complications of day-time somnolence, obesity, hypertension and eventual risk of cor pulmonale.
●Cardiac abnormalities – affecting 40-60% children, typically AVSD (20% of Down’s children, and 25% of AVSD diagnoses).
●Respiratory – recurrent chest infections due to silent aspiration and impaired immune function, specifically cellular immunity.
●Gastrointestinal – 7% of children with have GI tract abnormalities including oesophageal atresia or trachea-oesophageal fistula, duodenal atresia and imperforate anus. Slight increase in Hirschsprung’s, but typically worse outcomes of those affected.7
●Musculoskeletal – Hypotonia, particularly in the neonatal period, often manifesting with early feeding difficulty Increased risk of atlanto-axial dislocation, which needs to be considered in children presenting acutely with neck pain.
●Growth and Development–poor growth and short stature are common. There are separate ‘Down Syndrome’ growth charts available. Developmental delay is universal but variable; although some children may eventually live independently and gain employment, skills are likely to be acquired at a slower rate, in particular gross motor and speech development. Despite the level of neurodisability and developmental impairment, children with Down Syndrome are often socially very able.

Fig 3. The front page of a growth chart used for children with Down Syndrome.
●Endocrine –increased risk of hypothyroidism.
●Haematological – unique to this syndrome is Transient Myeloproliferative Disorder (TMD), affecting 5-30% of neonates. As the name suggests this is transient, usually correcting within 3 months. There is a subsequent increase in the risk of acute myeloid leukaemia.
Differential Diagnosis
Antenatal testing identifies risk of trisomies 13, 18 & 21 – Patau, Edwards’ and Down. Phenotypically these are distinctive from each other. Once a trisomy has been identified further tests (G-banded analysis) confirms trisomy 21.
It is important to carefully examine for features of Down syndrome when a related diagnosis is identified in order to differentiate whether these are distinct or part of a syndrome.
Investigations
Where there is antenatal diagnosis or high clinical suspicion, genetics need to be confirmed in the early post-natal period. The DSMIG outline appropriate course of action for initial management of a neonate with Down Syndrome. Much of the management is routine for all newborns, such as full new born examination, ensure meconium and urine has been passed and review of feeding, however care needs to be conducted with a higher index of suspicion based on anticipated problems.
Early Management includes:
● Senior paediatrician and midwife to attend to the family. A new educational initiative by Down Syndrome Association ‘Tell it Right, Start it Right’ urges those managing these families to have the correct and most up-to-date information in the early counselling phase.8
● Blood tests: QF-PCR test, followed by G-banded analysis to identify trisomy 21. Full Blood Count and blood film (DSA neonatal)
● Newborn eye assessment
● Universal Newborn Hearing screen
● Guthrie test – new born blood spot on day 5 to screen for congenital hypothyroidism
● Electrocardiography and echocardiography
Management
Down syndrome children are managed by a multi-disciplinary team, whose care is normally coordinated by a community or neurodisability paediatrician. Families will receive a ‘personal child health record’ (PCHR) as an additional insert for ‘The Red book’ which has condition specific information with which to guide their care. Other specialty input is dictated by associated comorbidities, for example by cardiology, ENT or respiratory physicians and surgeons. The overall aim is to treat any associated conditions, promote health and development, and reduce any disability or functional limitation. A routine schedule is advised by the Down Syndrome Medical Interest Group (www.dsmig.org.uk). This is a systems approach to identify possible growth delay, respiratory or cardiac problems and investigation of thyroid function and an audiology assessment. See Figure 3.
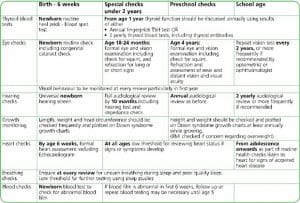
Fig 4. Recommendations for Medical Surveillance essentials for all children with Down Syndrome, available at: www.dsmig.org.uk
Where families are planning subsequent pregnancies genetic counselling is offered, and karyotype analysis would be performed to indicate risk to future off spring.
Complications
Life expectancy is slightly reduced at 60 years and there continues to be increased morbidity in later life, in particular increased incidence of Alzheimer’s dementia.
References
| No. | Reference |
| 1 | Harris W. Fourth Edition Examination Paediatrics. Elsevier Australia 2012 Chapter 9: Genetics and Dysmorphology p 253-265. |
| 2 | Wu J, Morris JK (2013); Trends in maternal age distribution and the live birth prevalence of Down’s syndrome in England and Wales:1938-2010. Eur J Hu Genet 21 (9): 943-947 |
| 3 | Manchester Centre for Genomic Medicine. Lab services >Down Syndrome. Available ONLINE AT: http://www.mangen.co.uk/lab-services/view-details.php?tag=109 Accessed on: 4/06/2017 |
| 4 | NHS Choices. Causes of Down Sydrome. Last reviewed: 30/04/2017 Available ONLINE at http://www.nhs.uk/Conditions/Downs-syndrome/Pages/Causes.aspx Accessed on: 30/05/2017 |
| 5 | NHS Choices. Pregnancy and Baby Down Syndrome. Last reviewed: 09/02/2015 Available ONLINE at: http://www.nhs.uk/conditions/Downs-syndrome/Pages/Introduction.aspx#screening Accessed on: 30/05/2017
|
| 6 | RCOG. Non-invasive Prenatal testing for Chromosomal Abnormality using maternal plasma DNA. Scientific Impact Paper No.15. March ’14. |
| 7 | DSMIG Best Practice Guidance – Neonatal. Basic Medical Surveillance Essentials for Children with Down Syndrome- Final DRAFT version. November 2016. Available ONLINE at: https://www.dsmig.org.uk/information-resources/guidance-for-essential-medical-surveillance/ Accessed on: 30/06/2017 |
| 8 | Down Syndrome Association. Antenatal, neonatal and postnatal care Guide for Practitioners. Aug 22, 2015. Available ONLINE at: https://www.downs-syndrome.org.uk/download-package/antenatal-neonatal-postnatal-care-guide-for-practitioners-2015/ Accessed on: 6/07/2017 |

