Croup, also known as acute laryngotracheitis or acute laryngotracheobronchitis (2), is a common viral childhood illness. It presents with a harsh barking cough and other clinical features including including stridor, hoarseness of voice, and fever.
In this article, we will discuss the epidemiology, pathophysiology, clinical features and management of croup.
Epidemiology
- Commonly affects children who are aged 6 months – 3 years, but can affect those who are as young as 3 months (1)
- Peak incidence is at 2 years of age (1)
Pathophysiology
Croup is a viral upper respiratory tract infection which results in mucosal inflammation anywhere between the nose and trachea (2,5). The most common organism is the parainfluenza virus; further organisms are given in the table below (2).
The characteristic barking cough of croup is caused by the impaired movement of the vocal cords.
| Causative Organisms |
| – Parainfluenza Virus (types I,II, II & IV)
– Respiratory Syncytial virus – Adenovirus – Rhinovirus – Enteroviruses – Measles – Meta Pneumovirus – Influenza A and B – Mycoplasma pneumoniae (rare) (2) |
Risk Factors
- Being Male
- male:female incidence ratio of 1.43:1 in <6 month children & 1.73:1 in children aged 6 to 12 months
- Autumn & Spring Season
- C/C variant of the CD14 C-159T gene has been shown by genetic studies to have a lower prevalence of croup (2).
Clinical Features
| From History | From Examination |
| – Typically a 1 to 4 day history of non-specific cough, rhinorrhoea and fever, progressing to a barking cough & hoarseness
– Symptoms are worst at night – Other symptoms: fever – Red Flag symptoms for respiratory failure: drowsiness, lethargy (2) |
– Stridor
– Chest sounds may be normal, but if there is a severe airflow limitation these sounds can be decreased – If in respiratory distress: tachypnoea, intercostal recession – Red Flag signs for respiratory failure: cyanosis, lethargic/decreased level of consciousness, laboured breathing, tachycardia (1,2)
|
The presenting symptoms vary according to the severity of disease which can be determined using the Westley Croup Score.
Westley Croup Score
The Westley Croup Score provides a valid scoring system that helps to categorise children based on their presenting clinical features:
| Clinical feature | Score |
| SaO2 <92% | 0 = None
4 = When agitated 5 = At rest |
| Stridor | 0 = None
1 = When agitated 2 = At rest |
| Retractions | 0 = None
1 = Mild 2 = Moderate 3 = Severe |
| Air entry | 0 = Normal
1 = Reduced 2 = Markedly reduced |
| Consciousness | 0 = Normal
5 = Reduced |
Westley Croup Score
Once calculated, children can be categorised into 1 or 4 levels of severity:
Mild (score 0-2)
Moderate (score 3-5)
Severe (score 6-11)
Impending respiratory failure (score 12-17)
Differential Diagnosis
- Epiglottitis (see table to differentiate from croup, 5)
- Inhaled foreign body
- Inhaled noxious substance
- Acute anaphylaxis
- Bacterial tracheitis
- Diphtheria
- Laryngomalacia or another congenital cause of upper airway stenosis (eg, aortic arch abnormality causing external airway compression)
- Peritonsillar abscess (quinsy)
- Retropharyngeal abscess
- Angioneurotic oedema
- Laryngeal mucosal lesions such as laryngeal web, papillomata and haemangioma
- Vocal cord paralysis (2)
| Croup | Epiglottitis | |
| Time Course | Days | Hours |
| Features Prior | Coryza | None |
| Cough | Barking | Slight if any |
| Feeding | Can drink | No |
| Mouth | Closed | Drooling Saliva |
| Toxic | No | Yes |
| Fever | <38.5 degrees | >38.5 degrees |
| Stridor | Rasping | Soft |
| Voice | Hoarse | Weak or Silent |
Investigations
Diagnosis is normally a clinical decision.
For any additional tests it is important to consider the distress that these could cause the child.
Laboratory tests: FBC, CRP, U&Es
Imaging or invasive tests:
- Chest X-Ray: To identify other possible causes of symptoms including inhaled foreign bodies.
- Direct or indirect laryngoscopy is not usually performed unless the illness is atypical or another cause of airway obstruction is suspected.
Other: pulse oximetry
Risk scoring (if relevant): See mild, moderate, severe classification above
Management
Location of care
Most children with mild croup can be managed at home but consider admission in the following cases: (1)
- Previous history of severe airway obstruction
- < 6 months of age
- Immunocompromised
- Have had inadequate fluid intake
- Have had a poor response to initial treatment
- The diagnosis is uncertain
- There is significant parental anxiety
Advice to parents for home-managed patients should include: (1)
- Explaining that the symptoms usually resolve within 48 hours but may last for up to a week.
- Explaining that croup is a viral illness and antibiotics are not needed.
- Paracetamol or ibuprofen can be used to control pain and fever.
- Ensure that the child has an adequate fluid intake.
- To seek urgent medical advice if symptoms worsen e.g. the development of intermittent stridor at rest or if the child starts to have a high fever and heart rate (this could indicate a different diagnosis such as bacterial tracheitis).
- To call an ambulance if the child starts to show signs of respiratory failure.
Immediate hospital admission should occur if: (1)
- The child has moderate/severe croup or impending respiratory failure.
- You suspect a serious disorder caused by infection e.g. peritonsillar abscess, laryngeal diphtheria, or a non-infectious cause e.g. foreign body, angioneurotic oedema.
Treatment:
- For all children with croup give a single dose of oral dexamethasone (0.15mg/kg body weight) or oral prednisolone (1-2mg/kg body weight) (1).
- Nebulised adrenaline can be given to provide temporary relief of symptoms (5).
- Ensure the child is kept as calm as possible as continuing crying increases oxygen demand & causes respiratory muscle fatigue (2).
- Humidified air/steam inhalation is not advised (2).
- Oxygen Therapy as required.
- Contact ENT and an anaesthetist if there is need for airway support (5).
Complications
Complications are rare and the majority of children do not need hospitalisation. In children that are intubated the mortality rates are less than 0.5% (2)
- Lymphadenitis
- Otitis Media
- Dehydration, as a consequence of not being able to maintain fluid intake (2)
- Rare: Bacterial superinfection resulting in pneumonia or bacterial tracheitis
- Extremely rare: Pulmonary oedema, pneumothorax
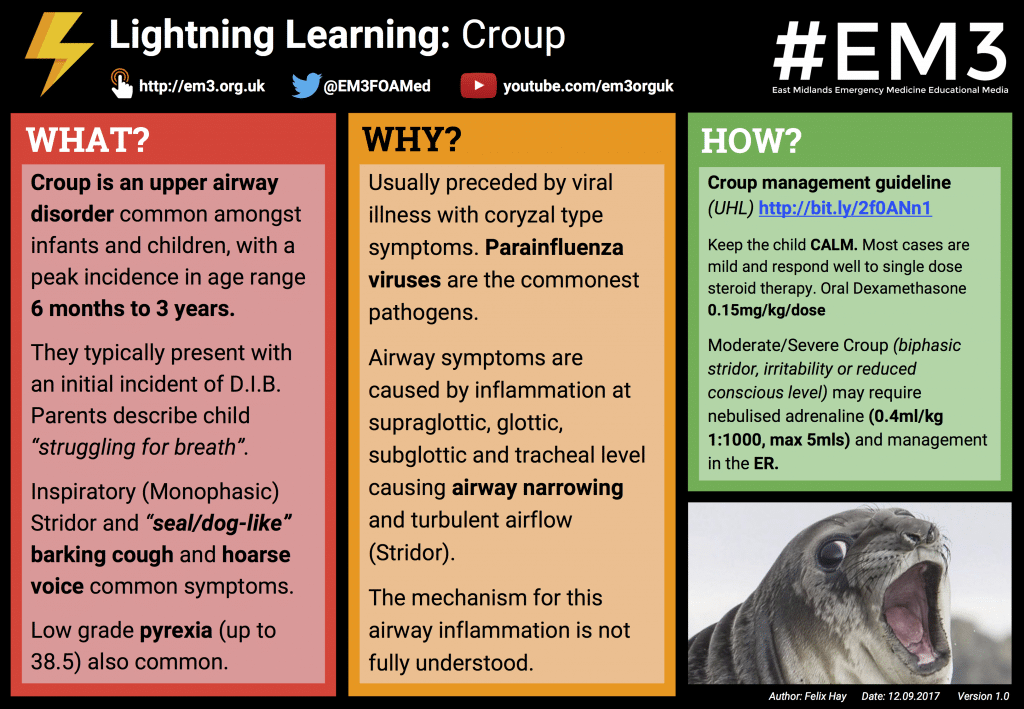
Lightning Learning
Thanks to the team at www.em3.org.uk we now have a ‘Lightning Learning’ resource for you to take away.
References:
| (1) | NICE Clinical Knowledge Summary Croup: http://cks.nice.org.uk/croup#!topicsummary – 11/09/16 |
| (2) | http://patient.info/doctor/croup-pro -11/09/16 |
| (3) | Paediatrics at a glance 3rd Edition 2012 |
| (4) | Crash Course Paediatrics 3rd Edition 2008 |
| (5) | Oxford Handbook Paediatrics 3rd Edition 2013 |
| (6) | Kumar and Clark’s 8th Edition 2012 |
