Diabetic Ketoacidosis (DKA) is a metabolic emergency occurring in Type 1 Diabetes Mellitus (T1DM). It is characterised by:
- Acidosis: Blood pH below 7.3 or plasma bicarbonate below 15mmol/litre AND
- Ketonaemia: Blood ketones (beta-hydroxybutyrate) above 3mmol/litre
- Blood glucose levels are generally high (above 11mmol/litre), although children with known Type 1 diabetes can less commonly develop DKA with normal blood glucose levels
These diagnostic criteria are stated by the British Society of Paediatric Endocrinology and Diabetes guideline for DKA management (1). DKA can be life threatening. The three complications which account for the majority of deaths in these children are cerebral oedema, hypokalaemia and aspiration pneumonia.
An understanding of the principles discussed in the ‘Approach to the Seriously Unwell Child’ article, combined with the knowledge from the BSPED guidelines, will help you manage these children appropriately.
Epidemiology
Prevalence rates of T1DM in children has remained stable since 2013, with an incidence of 24.5 per 100,000 general population (2).
In established T1DM, the risk of DKA is 1–10% per patient per year (3). Reported mortality rates from DKA in children in the UK are around 0.3%, with the majority secondary to cerebral oedema (4)
Pathophysiology
Understanding T1DM can seem overwhelming at first but once you have a clear understanding of the pathophysiology, this makes clinical features and management principles much easier to make sense of. The process which occurs in T1DM is explained below:
- T1DM is best seen as ‘starvation in the midst of plenty,’ where blood glucose levels are raised as it cannot be used for metabolism or stored due to an absolute deficiency of insulin (caused by autoimmune destruction of pancreatic beta cells).
- This leads to a rise in counter-regulatory hormones including glucagon, cortisol, catecholamines and growth hormone.
- The increase in these gluconeogenic hormones not only raises the blood glucose concentration further, but also leads to accelerated break down of adipose (fatty) tissue, resulting in rising levels of acidic ketone bodies (beta-hydroxybuturate).
- The hyperglycaemia and subsequent glycosuria causes an osmotic diuresis and the patient becomes polyuric, resulting in dehydration.
- Vomiting is common in DKA and further compounds the dehydration and stress, resulting in a perpetuating cycle of worsening acidosis and dehydration.
- Unless insulin is given, this process continues to spiral out of control and can be fatal.
The figure below summarises this information.
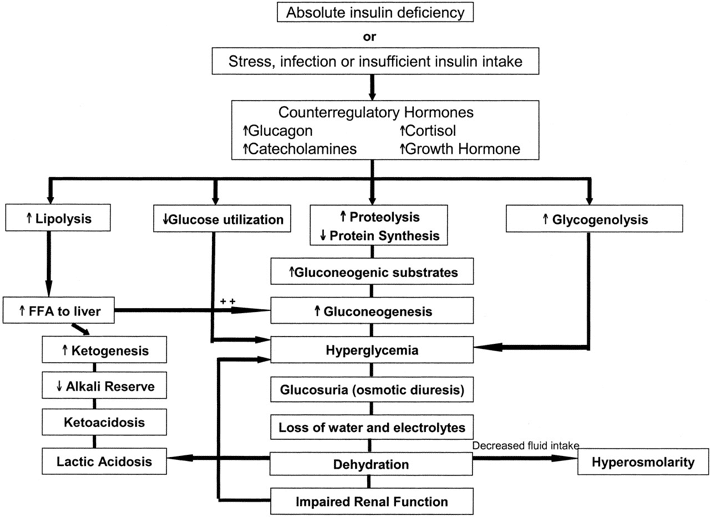
Figure 1 (5) Pathophysiology of DKA
Risk Factors
Although some children will be diagnosed with T1DM in the community at an early stage, most new diagnoses present in DKA to a local Emergency Department. For these new diagnoses, there may or may not be an intercurrent illness which has precipitated this. Children with known t1DM can also develop DKA for a variety of reasons:
|
Factor leading to DKA in known T1DM |
Examples |
| A lack of insulin | Non – compliance with insulin treatment
Device failure – pump or pen Changing insulin requirements during puberty |
| An excess of glucose | Increased ingestion of glucose |
| Intercurrent illness | Infection |
Clinical Features
History
A large systematic review in 2011 explored the presentation of T1DM in children and young adults with Diabetic Ketoacidosis (DKA) at diagnosis (6). Findings which are highly relevant when taking histories are:
- The mean duration of symptom before the child presented in DKA was 16.5 days.
- Up to 38.8% of children who presented with DKA had been seen by at least 1 doctor before diagnosis
These two figures are important because the child’s symptoms may often have been put down to another illness by the parent or GP and it is therefore important to explore these recent symptoms in more detail and have a low threshold for testing a bedside blood glucose in all unwell children.
The symptoms of DKA often include feeling generally unwell and lethargic, nausea and vomiting and abdominal pain. Early cerebral oedema may produce headache and irritability, progressing to confusion, drowsiness or collapse. There may also be symptoms of concurrent infection such as fever, cough, diarrhoea or dysuria.
If DM has not been previously diagnosed, the preceeding symptoms to establish from the history are those of:
- Weight loss – try to quantify this wherever possible
- Polyuria – this may also present as new night-time bed wetting in younger children
- Polydipsia
It is also useful to explore the family history of DM or other autoimmune conditions.
In known diabetic patients, ask specifically about their current insulin regimes and doses and their recent control. You should also establish a good insight into their overall diabetes management including their named consultant, clinic follow up and previous admissions.
Examination
Patients presenting in DKA often look very unwell. When performing a systematic ABCDE assessment look for the following features:
Signs of respiratory compromise
- Deep, sighing breathing (Kussmaul breathing)
- Tachypnoea
- Subcostal and intercostal recessions
Signs of circulatory compromise
- Shock – tachycardia, hypotension, increased capillary refill time and cool peripheries
- Dehydration – dry mucous membranes, sunken eyes/fontanelle and reduced skin turgor
Gastrointestinal signs
- Abdominal pain which may be severe and can mimic a surgical abdomen
Signs of neurological compromise
- Make an assessment of the patient’s conscious level (using AVPU or GCS) including ‘neuro-observations’, heart rate, blood pressure and pupillary response to light. Signs of cerebral oedema are irritability, slowing pulse, rising blood pressure and reducing conscious level.
- Papilloedema is a late sign.
Other
- Non-specific weakness, general malaise and ketotic breath which has a fruity, ‘pear drop’ smell
- Note that fever is not a feature of DKA. If present, suspect an underlying infection.
- Weigh the child wherever possible as this is useful when considering later fluid calculations.
Differential Diagnosis
- Hyperosmolar Hyperglycaemic State – this usually occurs in T2DM patients, especially when there are learning difficulties or other factors preventing proper hydration. These patients present with signs of hypovolaemia and marked hyperglycaemia but there is no ketone production or acidosis. Serum osmolality is usually 320mosmol/kg or higher.
- New presentation of T1DM, not in DKA
- Dehydration from another cause e.g. Gastroenteritis
- Sepsis – may also co-exist with DKA so have a high index of suspicion
- Appendicitis, intussusception or other causes of a ‘surgical abdomen‘
- Acidosis from another cause such as renal failure or substance ingestion (Salicylate toxicity).
Investigations
- Bedside blood glucose and ketones from finger prick. Urinary ketones can be used to diagnose DKA on a urine dipstick if blood ketone testing is not available, but obtaining urine samples from unwell, dehydrated patients can be difficult. They are also a delayed and indirect method of testing for ketones, indicating blood levels of ketones approximately four hours previously.
- Blood gas – A capillary or venous sample can be used and gives the acid-base balance as well as the electrolyte values.
- Laboratory samples for blood glucose, U&Es, FBC and creatinine should be sent at the time of cannulation. These may show acute renal impairment with a raised urea and creatinine.
- 12 lead ECG and cardiac monitoring for signs of hyper- or hypokalaemia
Interpreting the results
As stated previously, DKA consists of:
- Acidosis: Blood pH below 7.3 or plasma bicarbonate below 15mmol/litre AND
- Ketonaemia: Blood ketones (beta-hydroxybutyrate) above 3mmol/litre
- Blood glucose levels are generally high (above 11mmol/litre), although children with known Type 1 diabetes can less commonly develop DKA with normal blood glucose levels
The pH is further subdivided to give a DKA severity score and to determine the degree of assumed dehydration:
| DKA Severity | Threshold values | Dehydration |
| MILD | Venous pH 7.20-7.29 or bicarbonate <15mmol/litre | 5% |
| MODERATE | Venous pH 7.10-7.19 or bicarbonate <10mmol/litre | 7% |
| SEVERE | Venous pH less than 7.10 or bicarbonate <5mmol/litre | 10% |
Other tests may be considered depending on local guidelines and also the clinical condition of the patient. For example, some trusts advise taking all the ‘new diabetic bloods’ including autoimmune screen tests (HbA1c, thyroid function, coeliac screen). If you are suspecting intercurrent bacterial infection, consider cultures as appropriate (e.g. blood culture, urine dip/MC+S, throat swab, CSF culture etc). A chest radiograph may be needed if pneumonia is suspected.
It is important to note that unwell children and their concerned parents can find these acute situations with multiple investigations very upsetting. This is particularly crucial for first presentations of diabetes because these children will need repeated bloods as an inpatient, followed by a lifetime of blood sugar testing, insulin injections and outpatient clinics. Getting it ‘wrong’ the first time can have a devastating effect on this trust relationship and so making the experience as pleasant as possible from the offset is vital. This may mean involving a play specialist or using local anaesthetic cream during cannulation (if the child is stable enough to allow for this).
Management
The management of DKA in paediatric patients differs to that in adults. The main reason for this is that children are at a much higher risk of developing cerebral oedema in the rehydration phase of treatment. However, a recent study looking at fast vs slow rehydration in these patients provided further evidence to suggest that the risk of developing cerebral oedema does not appear to be related to IV fluid administration (7). The traditional cautious approach to fluid resuscitation in these children has thus been adapted to take account for this in many new guidelines.
The BSPED DKA Guideline (1) can be accessed online and gives a full description of the recommended management for this condition. This guideline includes examples of fluid regime calculations, which are particularly useful since these can be complex as the clinician must take into account fluid deficit and maintenance. BSPED have developed an online calculator to aid these calculations and create a personalised auditable pathway. However, we recommend that you write the steps of fluid calculation in the patient’s medical notes and use the calculator to double check. This allows others to understand the rationale behind your prescribing and guards against the input of incorrect numbers into the calculator. A summary of the key points of DKA management using this guideline is given below.
Assessment and emergency treatment
- Airway – Ensure that the airway is patent and consider intubation if there is reduced conscious level -this will involve contacting the anaesthetic and paediatric intensive care team.
- Breathing – Administer high flow oxygen via a non-rebreathe mask.
- Circulation – Most children in DKA will have signs of significant dehydration and poor peripheral perfusion. Only the sickest children will have signs of clinical shock. Clinical features of shock include tachycardia, increased central capillary refill time and hypotension as a late sign. There have been recent changes in the BSPED DKA management guidance which place greater emphasis upon restoring circulating volume in those children with shock, whilst balancing this against the risk of potentiating cerebral oedema. Initial fluid regimes are as follows:
| Children in shock | Children NOT in shock | |
| Initial bolus |
20mL/kg of 0.9% sodium chloride over 15 minutes |
10mL/kg 0.9% sodium chloride over 1 hour |
| Ongoing fluids |
Up to 40mL/kg total if ongoing shock before inotropes considered. DO NOT subtract from ongoing fluid calculation (deficit + maintenance) |
Calculate fluid deficit based on % dehydration. Subtract the initial 10mL/kg bolus from this and add maintenance |
- Disability – If there is a reduced conscious level or vomiting then insert an NG tube and leave on free drainage to prevent aspiration of stomach contents. Have a high index of suspicion for cerebral oedema if this is required.
- Expose – If there are signs of sepsis (fever/hypothermia, hypotension, refractory acidosis or lactic acidosis,) treat with IV antibiotics as per local guidelines.
The management of children in DKA should always be discussed with the responsible senior paediatrician.
Ongoing management
The BSPED guideline is an excellent summary of how to acutely manage DKA and should be followed step by step. Below, we have outlined some of the key principles to follow and given an example of a fluid calculation.
If the child is alert, not clinically dehydrated and not vomiting, it may be possible to treat DKA with oral fluids and subcutaneous insulin, even if blood ketones are very high. Most children however, will require the initiation of IV fluid replacement followed by the addition of an insulin infusion.
It is best to consider fluids required in these 3 groups:
- Resuscitation fluids: This describes any boluses given to patients with shock
- Deficit fluids: This is calculated from the assumed dehydration level based upon the pH at presentation. The initial 10mL/kg 0.9% sodium chloride given to those presenting without shock over the first hour is deducted from this
- Maintenance fluids: Whereas previously maintenance volumes were reduced for diabetic patients, these now follow normal maintenance fluids for children rules (100mL/kg/d for first 10kg; 50mL/kg/d for the next 10kg; 20mL/kg/day thereafter up to 80kg max). Check out our fluid management article for more information on maintenance fluids in paediatrics
The fluid to use after initial bolus fluids is 0.9% sodium chloride with 20mmol potassium chloride in each 500mL bag. This will likely need adjusting based on the patient blood glucose level. You should not give oral fluids to a patient receiving IV fluids for DKA (mouth rinses are acceptable for comfort).
Starting fluid rate = Deficit + Maintenance
Over 48 hours
Case example: You are asked to prescribe fluids for a 5 year old boy weighing 20kg who is in DKA with a pH of 7.2. He has NO clinical features of shock. His potassium level is 4.
1. Resuscitation fluids:
Not indicated (no shock)
2. Deficit fluids:
Initial bolus 10mL/kg over 1 hour = 200mL
pH 7.2 = mild DKA therefore 5% dehydration correction
5(%) x 20 (kg) x 10 = 1000mL
Subtract initial bolus from deficit:
1000-200 = 800mL
Replace over 48 hours:
800/48 = 17mL/hr
3. Maintenance fluids:
100mL/day for 1st 10kg = 1000mL
50mL/day for next 10kg = 500mL
Total = 1500mL = 63mL per hour over 24 hours
Total fluid requirements: 17 + 63 = 80mL per hour
Fluid choice: 0.9% sodium chloride 500mL bag with 20mmol KCL
IV Insulin:
Insulin should be delayed for 1-2 hours after beginning IV fluid therapy as this has been shown to reduce the chance of cerebral oedema. A dose of 0.05 – 0.1 units/kg/hour of a soluble insulin such as Actrapid is usually sufficient. Blood glucose should be checked hourly and ketones every 1-2 hours. If the patient is a known T1DM presenting in DKA, they should continue their regular long acting subcutaneous insulin during DKA management.
Potassium replacement:
In patients with DKA, there is a depletion of total body potassium. Gluconeogenic hormones cause potassium to be transported out of cells and into the blood, where they are then lost in the urine as part of the osmotic diuresis. It is therefore vital to replace and monitor potassium levels as part of the treatment of DKA which is why initial fluid regimes contain potassium. However, very dehydrated patients not producing any urine (possible acute kidney injury) may have potassium levels at the upper end of normal or high at presentation. In these patients, do not administer potassium until urine has been passed or repeat levels have been taken.
ECG monitoring should continue throughout treatment in order to look for cardiac signs of hyper and hypokalaemia.
Stabilisation and continued care
Children in DKA require one to one nursing. Vital nursing observations include strict fluid balance monitoring and hourly observations with BP and GCS.
Regular reviews by the medical team should include repeated blood glucose, ketones, blood gas and U&Es. The results of these guide further fluid and insulin management – please see the full guideline for details.
Oral fluids can be commenced once ketosis is resolving and there is no nausea of vomiting.
DKA is considered to be resolved once the child is clinically well, drinking and tolerating food and the blood ketones are less than 1mmol/litre or pH is normal. Subcutaneous insulin can then be started and IV insulin stopped one hour later.
Further care then involves liaising with the diabetic team regarding patient (and parent) education and planning towards discharge.
Complications
Cerebral Oedema:
This is the leading cause of death in children presenting with DKA and occurs in up to 1% of cases with a 20-25% mortality (8).
Careful and regular observation of neurological status should be documented. Headache, confusion, irritability, increasing drowsiness, hypertension with bradycardia and focal neurological signs such as cranial nerve palsies and papilloedema are all signs suggestive of cerebral oedema.
Hypokalaemia:
Life threatening arrhythmias can occur as a result of potassium depletion. Figure 2 shows ECG features associated with hypokalaemia.
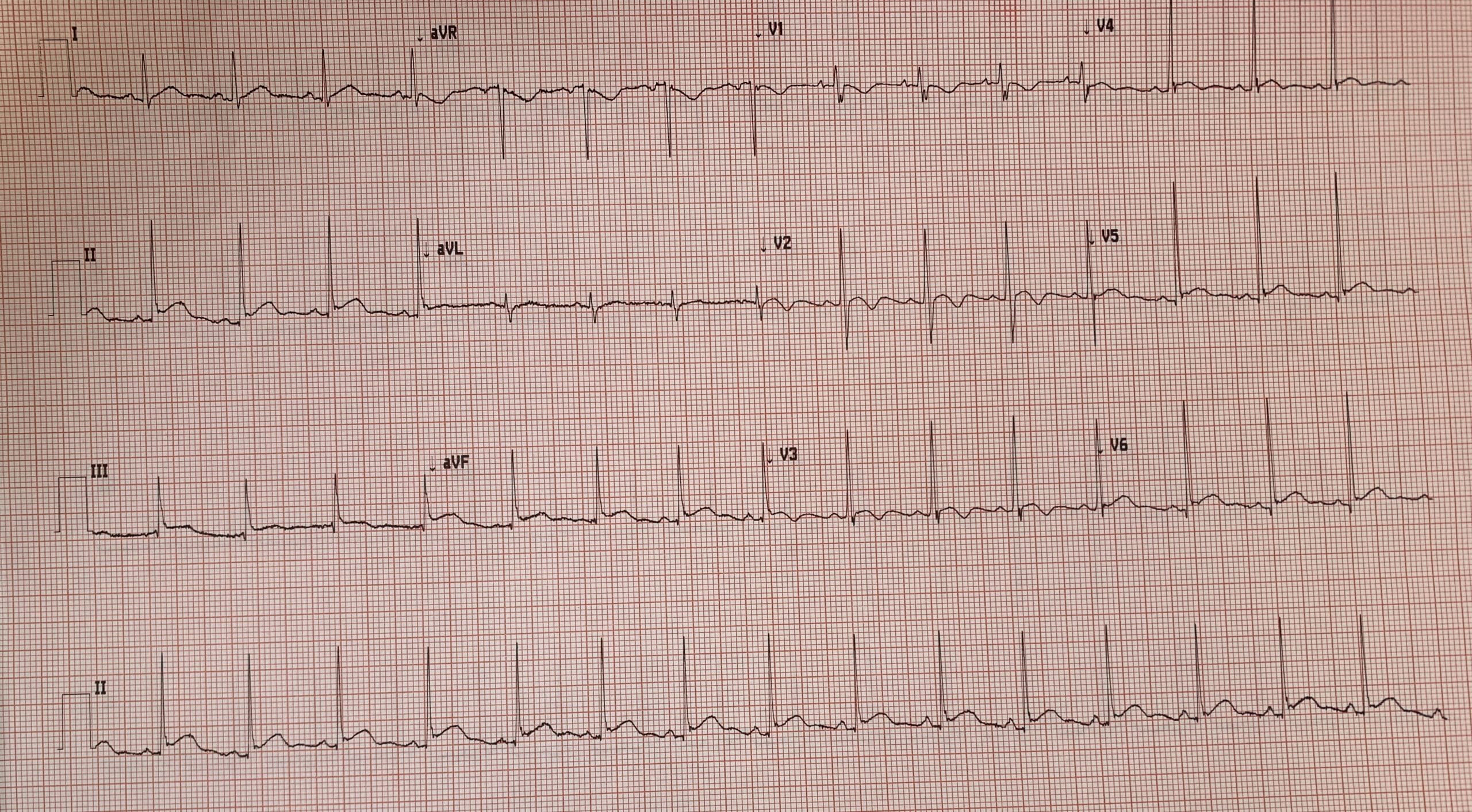
Figure 2: ECG features associated with hypokalaemia (U wave and T wave inversion leads V1-V3). This patient had a potassium of 2.0
Regular blood tests are required during treatment and the child should be monitored for cardiac changes. If the hypokalaemia is severe the insulin infusion may need to be reduced or stopped temporarily.
Central venous access may be required in order to give more concentrated solutions of potassium chloride (>40mmol/L).
Aspiration Pneumonia
Children with a reduced conscious level are at high risk of aspirating, especially those with an associated ileus or gastric paresis, which can lead to an aspiration pneumonia. NG tube insertion in these patients helps reduce the risk.
Hypoglycaemia
Blood glucose level should be monitored closely when giving IV insulin as the blood glucose can fall rapidly, causing hypoglycaemia. Rehydration fluids should be changed to include glucose once blood glucose falls to 14mmol/l to prevent this.
Prognosis
The majority of children who present in DKA will recover well and be discharged home within a few days. However, it is the ongoing education and support from the diabetic multidisciplinary team as well as the engagement from the child and family which will have the largest impact on their future diabetic control.
References
| (1) | BSPED Interim Guideline for the Management of Children and Young People under the age of 18 years with Diabetic Ketoacidosis 2020. Accessed via: https://www.bsped.org.uk/media/1798/bsped-dka-guideline-2020.pdf |
| (2) |
RCPCH: National Paediatric Diabetes Audit: Annual report 2018-19 Care Processes and Outcomes. Accessed via: https://www.rcpch.ac.uk/sites/default/files/2020-03/final_npda_core_report_2018-2019.pdf |
| (3) | Wolfsdorf J, Craig ME, Daneman D, et al. Diabetic ketoacidosis, ISPAD Clinical Practice Consensus Guidelines 2006–2007. Pediatr Diabetes 2007;8:28-43. |
| (4) | Dunger DB, Sperling MA, Acerini CL, et al. ESPE/LWPES consensus statement on diabetic ketoacidosis in children and adolescents. Archives of Disease in Childhood 2004;89:188-194. |
| (5) | Diabetic ketoacidosis in infants, children, and adolescents: A consensus statement from the American Diabetes Association. Diabetes Care. 2006 May;29(5):1150-9. Wolfsdorf J1, Glaser N, Sperling MA; http://care.diabetesjournals.org/content/29/5/1150.long#F1 |
| (6) | Juliet A Usher-Smith et al. Factors associated with the presence of diabetic ketoacidosis at diagnosis of diabetes in children and young adults: a systematic review. BMJ 2011:343:d4092. |
| (7) | Kuppermann N, Ghetti S, Schunk JE, Stoner MJ, Rewers A, McManemy JK, Myers SR, Nigrovic LE, Garro A, Brown KM, Quayle KS. Clinical trial of fluid infusion rates for pediatric diabetic ketoacidosis. New England Journal of Medicine. 2018 Jun 14;378(24):2275-87. |
| (8) | Edge JA, Hawkins MM, Winter DL, Dunger DB. The risk and outcome of cerebral oedema developing during diabetic ketoacidosis.Arch Dis Child.2001;85 :16– 22 |
Authors:
1st Author: Dr Hannah Clark
Senior Review: Dr Jennifer Mann (Paediatric Emergency Medicine specialist registrar)
