Lymphoma is a malignancy of the lymphatic system. It is commonly divided into Hodgkin’s lymphoma and non-Hodgkin’s lymphoma. The term “non-Hodgkin’s lymphoma” encompasses a broad range of diagnoses, but it is not necessary for most students (aside from budding haematologists, perhaps!) to know about them in greater detail.
Epidemiology
Lymphoma accounts for over 10% of childhood cancers, although childhood cancer is in itself rare. Lymphoma is seen more commonly in boys than girls and is much more common in older children. Just over half of childhood lymphoma cases are non-Hodgkin’s lymphoma.
Pathophysiology
As with many malignancies, and particularly malignancies in children, the pathophysiology of lymphoma is not well understood. Development is multi-factorial, with infection, genetic factors and environmental exposures all potentially involved. In adults, lifestyle factors such as obesity, smoking and alcohol intake are all associated with increased lymphoma risk but it is less clear what, if any, part they play in the development of childhood disease.
Risk Factors & Clinical Features
History
Epstein-Barr Virus has been particularly implicated in the development of lymphoma. Immunosuppressed patients (eg those who have had a solid organ transplant) and those who have been treated for other cancers in the past are also at increased risk of lymphoma.
Lymphoma may present with a visible or palpable mass. There may be a history of “B symptoms” such as:
- Weight loss
- Night sweats
- Fevers
Other, more non-specific symptoms of malignancy, such as lethargy and anorexia, may also be present.
On Examination
Non-tender lymphadenopathy is the most common examination finding, however this may not necessarily be visible or palable, for example if mediastinal or intra-abdominal lymph nodes are involved. Mediastinal lymphadenopathy may present with cough, wheeze or other difficulty in breathing, and occasionally superior vena cava obstruction or airway compromise can occur.
Differential Diagnosis
The most common differential for a patient presenting with lymphadenopathy is reactive lymphadenopathy. There is likely to be a history of recent infection. If the lymph nodes themselves have become infected (lymphadenitis) they are likely to be tender and potentially fluctuant if an abscess has formed.
Leukaemia can also present with “bulky” disease and should be considered in patients with lymphadenopathy associated with signs and symptoms of anaemia and/or thrombocytopenia (see article on leukaemia).
Lymphadenopathy can also be a sign of metastatic malignancy from another site, but this is far more common in adults than children.
Investigations
Laboratory tests
Blood tests such as full blood count may be done to help diagnose differentials such as infection. Urea and electrolytes are also important as tumour lysis syndrome can occur before treatment begins in lymphomas with rapid cell turnover. LDH (lactate dehydrogenase) levels are usually elevated.
Imaging
USS of the area can help identify other nodes, and assists with biopsy.
Chest x-ray may be required if there are symptoms of mediastinal node involvement.
A full body CT to determine extent of disease (and therefore staging) is also required.
Biopsy
Lymph node biopsy is necessary for definitive diagnosis.
Risk scoring
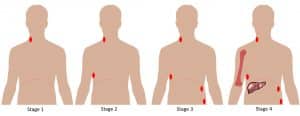
Lymphoma is staged according to how many groups of lymph nodes or organs are involved:
- Stage 1: Disease is present in a single group of lymph nodes or a single organ
- Stage 2: Disease is present in 2 or more groups of lymph nodes or organs on the same side of the diaphragm
- Stage 3: Disease is present in lymph nodes or organs on both sides of the diaphragm
- Stage 4: There is diffuse involvement of lymph nodes and organs such as the liver and bones
The presence of “B symptoms” is associated with worse prognosis at all stages and a B is added to any stage if these are present (eg stage 1B, 2B etc).
Management
Immediate
The presence of a mediastinal mass with potential airway compromise is an emergency. Treatment is with high dose steroids and airway support if required.
Superior vena cava obstruction (SVCO) may require stenting of veins to keep them patent, although it will usually resolve with treatment of the underlying malignancy.
If there is suggestion of tumour lysis syndrome, then hyperhydration is important. Allopurinol or rasburicase are also used.
Definitive and Long‐term
Treatment is with chemotherapy and possibly radiotherapy, depending on the stage of disease.
Prognosis and Complications
The majority of children and young people with lymphoma will recover completely, with Hodgkin’s lymphoma carrying a more favourable prognosis than non-Hodgkin’s lymphoma.
Complications include tumour lysis syndrome, which is seen when rapid lysis of tumour cells causes release of large amounts of phosphorus, potassium and calcium leading to potential kidney damage. This is most likely to occur when chemotherapy is first commenced, but may occur beforehand. Other complications are more generally related to cancer treatment and include neutropenia, alopecia and sub-fertility.
All children who are treated for cancer will have life-long follow-up to assess for late-effects of cancer treatment.
References
| (1) | National Registry of Childhood Tumours/Childhood Cancer Research Group http://www.ccrg.ox.ac.uk/datasets/registrations.shtml accessed 20/02/2017 |
| (2) | http://www.cancerresearchuk.org/health-professional/cancer-statistics accessed 20/02/2017 |
| (3) | PINKERTON, R., CAIRO, M.S. and COTTER, F.E., 2016. Childhood, adolescent and young adult non-Hodgkin lymphoma: State of the science. British journal of haematology, 173(4), pp. 503-504. |
1st Author: Dr Amanda Friend
Senior reviewer: Dr Carmen Soto (Senior academic paediatric registrar)