Paediatric palliative medicine is the medical care of children suffering from conditions that will limit their lifespan, particularly those who are not expected to survive beyond childhood.1
Definition
Together for short lives defines paediatric palliative care further
“An active and total approach to care, from the point of diagnosis or recognition, throughout the child’s life, death and beyond. It embraces physical, emotional, social and spiritual elements and focuses on the enhancement of quality of life for the child or young person and support for the family. It includes the management of distressing symptoms, provision of short breaks and care through death and bereavement”
Categories of Life Limiting Conditions
Life Limiting Conditions (LLC) are conditions for which there is no reasonable hope of cure and from which children or young people will die and include life-threatening conditions for which curative treatment may be feasible but can fail. Together for short lives recognises that four broad categories of life-threatening and life-limiting conditions may be delineated. Categorisation is important for the purpose of planning and needs assessment.
| Category | Example | ||
| 1 | Life-threatening conditions for which curative treatment may be feasible but can fail | Access to palliative care services may be necessary when treatment fails or during an acute crisis, irrespective of the duration of threat to life. On reaching long-term remission or following successful curative treatment there is no longer a need for palliative care services. | Cancer |
| 2 | Conditions where premature death is inevitable | There may be long periods of intensive treatment aimed at prolonging life and allowing participation in normal activities. | Cystic Fibrosis
Duchenne Muscular Dystrophy |
| 3 | Progressive conditions without curative treatment options | Treatment is exclusively palliative and may commonly extend over many years.
|
Batten Disease
mucopolysaccharidoses |
| 4 | Irreversible but non-progressive conditions causing severe disability, leading to susceptibility to health complications and likelihood of premature death | Children have complex health care needs and are at high risk of an unpredictable life-threatening event or episode. | Cerebral palsy
Spinal cord injury |
Despite falling mortality rates, the number of children living with LLCs is rising; this reflects general advances in medical care and preventative measures. There are in excess of 49,000 children and young people under 19 years in the UK living with a life-limiting or life-threatening condition that may require palliative care services. These conditions consist of an extremely diverse array of conditions (over 300) however up to 15% of patients requiring palliative care do not have a definitive underlying diagnosis2.
Children requiring palliative care services may have widely varying needs, as many have severe disabilities and multiple complex health and care needs. A child’s condition may lead to a palliative care approach being used exclusively or used in conjunction with curative treatments.
Palliative care services may be required at any point. They may start antenatally and continue beyond a child’s 18th birthday. Services may potentially be required from diagnosis or recognition, through active treatment, including that aimed at cure, to end of life care and bereavement4.
Location
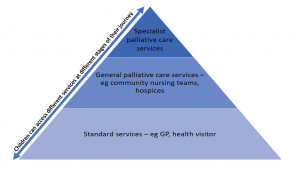
Children’s palliative care is delivered by a multitude of different providers, including primary, secondary and tertiary services, community services and hospices. All paediatric specialities may encounter children with palliative care needs whether an acute speciality or community. Effective networking arrangements between services, with good communication and care coordination is essential for successful paediatric palliative and end of life care.
Currently a large proportion of children die in hospital especially intensive care. Furthermore, due to lack of advanced planning, local services and skills a significant proportion of children with life limiting conditions invariably experience frequent, often prolonged hospital stays, usually within the paediatric unit or intensive care setting; effective palliative care services can help reduce this.
Child vs Adult Palliative Care
Child services differ from adult in the following ways:
- The number of children who die is small compared with the number of adults
- Many of the conditions are extremely rare and diverse
- Many of the conditions are genetic, and therefore more than one child in the family may be affected
- Paediatric palliative care may be needed for only a few days, weeks or months, or may be delivered on and off for a number of years. Adult palliative care is focused predominantly in the end stages of disease
- Children have continuous physical, emotional and cognitive development throughout childhood. Palliative care strategies need to adapt and respond to each child’s changing levels of communication and their ability to understand
- Provision of education and play when a child is seriously ill is essential. This introduces an additional dimension which adds to the complexity of care provision5
Managing Symptoms
A child’s physical symptoms can be managed in different ways as highlighted in the infographic below, however there are common goals that need to be followed independent of the approach.
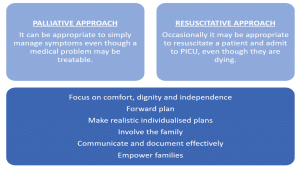
Fig 2 – Physical symptoms can be managed palliatively or with a resuscitative approach, but both with common goals
Looking after a child with palliative care needs may appear daunting and is likely to install an element of anxiety in the unexperienced doctor. However, remembering basic skills and following a logical approach goes a long way. It must also be remembered that there is much more to treating the terminally ill child than just symptom control; such as the emotional, social and spiritual needs of the child and those close to them.
The parents play a pivotal role in symptom control as they usually have the best understanding of the childs’s medical, nursing and social needs. It is vitally important that parents are involved in decision making and parents must feel that they have informed choice in the care of their dying child. This is very important in post bereavement support6.
It is beyond the remit of this article to discuss symptom management in detail however an excellent resource to utilise is the Basic Symptom Control in Paediatric Palliative Care document available from the together for short lives website –http://www.togetherforshortlives.org.uk/professionals/resources/request/2434 .
Advanced care planning
Advance care planning and clarity about resuscitation decisions are essential for effective quality palliative care. It involves discussions between the patient (where possible) and their care provider and often those close to them.
Advance Care Planning helps create advance statements about wishes and preferences such as preferred place of care, withdrawal of treatment and resuscitation status. It also helps in in decisions relating to care in the case of acute deterioration and may also address preferences for organ and tissue donation.
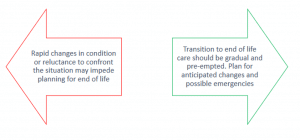
Care can be hindered by rapid changes but conversely enhanced by a smooth transition which is vital to successful care. Factors influencing the quality of care are outlined below:
Limitations of treatment
Children, young people and their families should be fully involved in decisions regarding their treatment including the difficult and emotive subject of withholding or withdrawing of life saving treatment. Their decisions should be recorded, visible and clear for all those involved in that patients care.
Do Not Attempt Resuscitation forms have been in existence for many years however there has been lots of controversy and misunderstanding over their design, use and limitations. In the era of increasing availability of children’s palliative care services and other support services the need for individualised recommendations for a person’s clinical care in emergency situations, including cardiorespiratory arrest is increasing.
The ReSPECT (Recommended Summary Plan for Emergency Care and Treatment) process supports the creation of these recommendations by initiating conversations to ensure a shared understanding of the condition, current issues and future outlook. The child’s/families preferences for care and realistic future emergency treatment are then explored.
The process is finalised by making and recording agreed clinical recommendations for the child’s care and treatment for future emergencies or deterioration7. These recommendations can be used by all practitioners involved in the patients care, whether in the home, community or hospital.
Ethical issues in paediatric palliative care
All ethical dilemmas require the consideration of the four fundamental principles –
- Autonomy – the right to self-determination
- Non-maleficence – the need to avoid harm
- Beneficence – the ability to do good
- Justice
Most ethical issues relate to end-of-life care and decision-making. The child’s inability to act autonomously and subsequent reliance on their parents often complicates resolving these dilemmas8.
When considering ethical issues within paediatric palliative care it is important to recognise the following points:
- Children represent a spectrum from the non-verbal infant to the fully conversant adolescent striving for independence and self-identity
- A child’s ability to make informed choices is not only dependant on their level of development but on their life experience
- Even young children have a right to be informed regarding decisions which affect their future
- As children acquire increasing competence, involvement in decision-making increases
- The Royal College of Paediatrics and Child Health advocate strongly for the participation of children in decision-making to the extent their ability allows
Summary
Paediatric palliative care comprises a comprehensive approach to treating the physical, psychosocial and spiritual needs of patients facing life-limiting illnesses and their families and requires the coordinated efforts of a large multidisciplinary team. This rapidly advancing speciality with ever increasing evidence base enters into all paediatric specialties and should be considered alongside active treatment for all children with life limiting or life threatening illnesses.
References
| (1) | RCPCH http://www.rcpch.ac.uk/training-examinations-professional-development/postgraduate-training/sub-specialty-training/paedi-10 |
| (2) | Fraser et al 2012 http://www.togetherforshortlives.org.uk/assets/0000/1100/Leeds_University___Children_s_Hospices_UK_-_Ethnicity_Report.pdf |
| (3) | http://www.togetherforshortlives.org.uk/assets/0000/4121/TfSL_A_Core_Care_Pathway__ONLINE_.pdf |
| (4) | NHS England https://www.england.nhs.uk/wp-content/uploads/2013/06/e03-paedi-med-pall.pdf |
| (5) | Together for short lives. http://www.togetherforshortlives.org.uk/professionals/childrens_palliative_care_essentials/approach |
| (6) | Together for short lives. http://www.togetherforshortlives.org.uk/assets/0001/4931/Symptom_Control_Manual_9.5_edition.pdf |
| (7) | ReSPECT. http://www.respectprocess.org.uk/ |
| (8) | The Royal Childrens Hospital Melbourne.Ethics. http://www.rch.org.au/rch_palliative/for_health_professionals/Ethics/ |
Authors:
First draft: Dr Claire Wastakaran
Senior review: Dr Anton Mayer (Paediatric palliative care consultant)